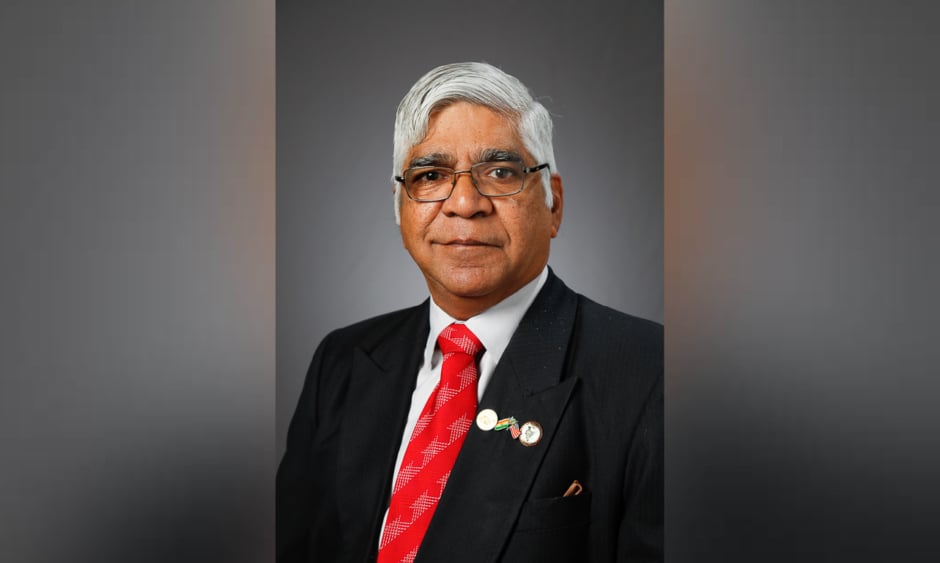
Dr Krishnan Ganapathy | Member of the Board of Directors of Apollo
Telemedicine Networking Foundation (ATNF) and Apollo
Telehealth Services; Past President Telemedicine
Society of India (TSI) and Neurological Society of India (NSI); Emeritus Professor at The Tamil Nadu Dr. M.G.R. Medical University, Chennai, India
![]()
At present, you are the President of the Apollo Telemedicine Networking Foundation (ATNF). What is the aim of ATNF, and how did you come to be involved with the Foundation?
It all started on the night of 16th September 1996, I had just finished delivering an institute lecture in the Indian Institute of Technology Kanpur (IITK), a globally recognised institution. Just after the question and answer session ended at 9 pm, Dr K. Srivathsan from the Department of Electrical Engineering at IITK, insisted I have dinner with him. He introduced me to the word ‘telemedicine’. Together, we prepared a project report from 11 pm to 4 am. I then commenced a love affair which over the last 24 years, has taken its toll. My legally wedded wife is often relegated to number three. Initially, I was wedded to neuro surgery and now it is telehealth. Having started the first stereotactic radiosurgery unit in South Asia, and as Secretary of the then 2,200-strong Neurological Society of India (NSI), conventional wisdom dictated that I should continue to focus my skills and energy completely on what I was trained for, namely neurosurgery. However, deep down was a nagging feeling: “Was there not something else which I could do to help more than a few thousand neurosurgical patients?” And then the story began. I took the road less travelled by and the rest, as they say, is history! In fact, I embarked on making geography, history, and distance meaningless!
Dr Prathap Reddy, Founder and Chairman of the Apollo Hospital Group, Chennai, India, visionary Nostradamus that he is, gave me a lot of support. On 24th March 2000, President Bill Clinton formally commissioned the world’s first Very Small Aperture Terminal-enabled village hospital in Aragonda in Andhra Pradesh (birthplace of Dr Reddy). In 2001, the Apollo Telemedicine Networking Foundation (ATNF) was formally established as a not-for-profit Section 25 company. Taking modern healthcare to remote areas using technology was the mission of ATNF. Between my neurosurgical commitments, I spent time and effort to help a skeleton staff of four full-time employees to achieve what in 2001 appeared preposterous: remote consultation! Every opportunity to put, then hardly existent, Indian telemedicine on the world map was utilised.
Which patients are set to benefit the most from the integration of telemedicine into health systems?
I honestly do not believe that there is one set of patients who will benefit more from the integration of telemedicine into the health system. In fact, there is not a single individual who would not benefit from remote healthcare. The very words ‘patient’ and ‘telemedicine’ may be inappropriate! I would prefer use of the words ‘telehealth’ and ‘beneficiary’. We should start promoting wellness, the eWay! Keeping everyone healthy remotely using technology is my mantra for the future. We can start by promoting health literacy. Providing dependable knowledge on a smartphone will lead to people’s empowerment and a reduction of preventable diseases. Under Ayushman Bharath, the world’s largest Universal Health Coverage for 500 million Indians, 150,000 telehealth enabled wellness centres will be functional throughout India. Theoretically, every single individual, healthy or sick, rich or poor, urban or rural, educated or not, can benefit in different ways through ‘contactless’ medicine. Physical distancing is here to stay. This should not be mistaken for social distancing or clinical distancing. Distancing is a term that should not exist for those deploying virtual healthcare, we are always there 24/7 on a small or large screen!
What are the challenges facing telemedicine today?
Perhaps in one way, the challenges facing telemedicine today are far less and can be addressed. When I first embarked on telemedicine 24 years ago, the very word was unfamiliar to most. It took a decade of intensive persistent evangelisation to create the semblance of an awareness. The second decade was spent in achieving a behavioural modification and technology acceptance among all stakeholders in the ecosystem. During the last four years, thanks primarily to public–private partnerships, revenue-generating business models have started to become available. The single most important challenge facing telemedicine is addressing the question, ‘WIIIFM: what is in it for me?’ WIIIFM is different for each stakeholder. The COVID-19 pandemic has made the entire globe realise that today, distance is meaningless. Physical distancing will be the norm. The world has turned upside down. I foresee that the challenge will no longer be to convince the healthcare provider and the beneficiary that telemedicine has advantages over face-to-face in person visits. Today, the challenge is to very quickly customise and make available a cost-effective, need-based, user-friendly, technologically efficient, and secure telehealth system which is compliant and adherent to newly formed regulations. The telemedicine system must be future ready and culturally sensitive. Insurance companies in India have already started recognising telemedicine for reimbursement. Revenue generation is critical for ensuring self-sustenance. Necessity is the mother of invention. Telehealth now has to take centre stage. It can no longer be lurking in the periphery. There is an opportunity in every crisis. The challenges facing us in introducing telemedicine are not insurmountable as there is a pressing need not tomorrow, not today, but yesterday. This universal demand alone makes all challenges pale into oblivion.
Teleradiology is thought of as one of the fastest moving fields in telemedicine. In your opinion, why do you think there has been a lot of progress in this area?
Imaging procedures are growing 15% annually against an increase of 2% in the radiologist population. Worldwide, there is a shortage of radiologists, particularly in subspecialties. The phenomenal additions to technology and cost reduction make it possible to have CT scans even in towns in India. Simultaneously connectivity in suburban and rural India is getting better. Radiologists, therefore, are extending their reach, some even to other continents! Telerad Tech (Bengaluru, India) provides 24/7 teleradiology services to 1,500 installations in 31 countries. This is particularly important when a subspecialist such as an MRI radiologist, neuroradiologist, paediatric radiologist, or musculoskeletal radiologist is needed. These subspecialists are generally only available in large metropolitan cities during daytime hours. Teleradiology allows for trained specialists to be available 24/7 in different time zones. We embarked on teleradiology only a few years ago. We set up 110 teleradiology centres in suburban and rural Uttar Pradesh, the largest state in India (population of 200 million), in the most challenging areas under a public–private partnership. Today, tens of thousands get imaging studies done without having to travel long distances.
You are reputed as having pioneered the introduction of telemedicine into India. What advice do you have for someone wanting to establish a telemedicine programme?
Be future ready. Learn from the mistakes of your predecessors. Remember that no telemedicine programme can be sustained unless it is revenue-generating. Technology is only a means to achieve an end not an end by itself. With more access to technology, do not forget that you are a doctor first and last. Tender, loving care can be bestowed virtually. Empathise and sympathise with your patient on the screen (small or big). Wipe their tears. Listen to them. Find out what they want. Answer all their queries. Technology is the least important. Context is critical. Stop a teleconsultation if your gut feeling suggests a face-to-face interaction. Adhere and comply with all changing regulations. We are in a stage of transition. All transitions offer great opportunities. Telemedicine, like medicine itself, is not black and white. It is still various shades of grey. Look back to 10th March 1876, when Alexander Graham Bell made the world’s first telephone call, a request for medical help, “Watson come here, I want you,” after having spilt battery acid on himself. We now have a diamond spoon in our mouths. COVID-19 is providing us with tens of thousands of virtual non-COVID-19 patients! You cannot ask for a more opportune time to start telemedicine. A strand of RNA 120 nm is your most efficient Chief Transformation Officer.
What impact has the COVID-19 pandemic had on the trajectory of the integration of telemedicine in day-to-day clinical practice?
Following notification of COVID-19 as a pandemic on 25th March 2020, the Ministry of Health for the Government of India notified Telemedicine Practice Guidelines for the country. This had been pending with the government for a long time. Because of uncertainty over whether practising telemedicine was legal in India, many doctors were not deploying it. Following this, several thousand doctors have attended orientation programmes conducted by the Telemedicine Society of India (TSI) and other organisations. I have personally given 29 webinars in the last 4 months on the role of telehealth in the present situation. Over 34,000 doctors have attended these sessions. One webinar was attended by 11,775 doctors. Another webinar (http://kganapathy.com/covid.html) was for eight countries and 808 attended. The interest has been unbelievable. Simultaneously, hundreds of hospitals in the public and private sectors are offering free teleconsultations for screening of COVID-19 patients. Health insurance companies have recognised telemedicine services for reimbursement. Contactless medicine is now being accepted. It appears that the ‘work from home’ culture will include doctors as well! The world has turned upside down. Delivery of healthcare services is being re-examined. In every crisis there is an opportunity. Telehealth is here to stay and will take centre stage after having been in the periphery for the last 24 years. There is no doubt whatsoever that in the last 4 months, developments in the face of COVID-19 have achieved what we could not for 24 years.
There is debate over the robustness of cybersecurity measures for patient data in telemedicine. What is your opinion on this?
We concede that privacy and security of patient data are very important. Yes, 200 million healthcare records have been reported to have been compromised in the USA alone. The later entry of India in using electronic medical records (EMR) has ensured that we don’t piggyback, we don’t even leapfrog (after all, how far can a frog leap!): we pole vault. Ethical, Legal and Social Issues (ELSI) guidelines regarding data ownership of EMR have been notified. Protected health information, data ownership, data access and confidentiality, EMR preservation, and patient-identifying information have all been addressed in great detail under existing Indian laws, including the Information Technology Act 2000 and its amendments. The stakeholders understand the importance of cybersecurity; however, sometimes I feel that we are getting paranoid about cybersecurity in healthcare. Yes, it is important but if we wait for a totally fool-proof secure system EMR and hospital information systems would never see the light of the day and the cost would be astronomical. Even the White House can be hacked! It depends how badly the hacker wants the information. I have always felt that there is a cultural difference between India and the West so far as hacking health records is concerned. We are not primarily a society that will litigate at the drop of a pin. Trust still is a part of our vocabulary.