The GISE Registry of Transcatheter Treatment of Mitral Valve Regurgitation (GIOTTO) is a prospective Italian registry designed to collect current, real-world procedural and clinical data on early and long-term outcomes of patients treated with MitraClip® (Abbott, Chicago, Illinois, USA) implantation. The enrolment started in February 2016 in 22 centres. From February 2016 to May 2018, 1,041 consecutive patients were enrolled in the 22 participating centres (66.4% males, n=622; mean age: 74.2±9.6 years); the target enrolment was 1,200 patients. The main aetiology was functional mitral regurgitation (FMR) (74.9%, n=780) and the remaining 261 patients (25.1%) had degenerative MR (DMR).
The majority of the cohort was highly symptomatic (New York Heart Association [NYHA] Class III [71.0%] or Class IV [11.6%]) and approximately 45.0% had coronary artery disease, 38.0% had a previous myocardial infarction, and 77.2% had a left ventricular ejection fraction <50.0%. About 65.0% of the patients had at least one episode of acute heart failure leading to hospitalisation within the previous 12 months, with a mean number of in-hospital days of 15.9±13.8.
The majority of patients >80 years old had DMR (60.9% versus 24.1% with FMR; p<0.001); 15% of patients exhibited mixed disease. Compared to FMR, patients with DMR were older (73±9 versus 79±9 years, respectively; p<0.001), with higher ejection fractions (32±10% versus 56±11%, respectively; p<0.001) and better clinical statuses (NYHA Class III and IV: 83.9% versus 74.4%, respectively; p=0.001). Device implantation was successful in 98.3% of patients, with MR graded ≤2 at discharge in 93.8% of patients. The mean procedural time was 1 hour and 10 minutes and the mean number of MitraClips implanted per patient was 1.75±0.7 (1 clip [35.6%], 2 clips [52.0%], 3 clips [10.7%], or 4 clips [0.9%]) (Figure 1).
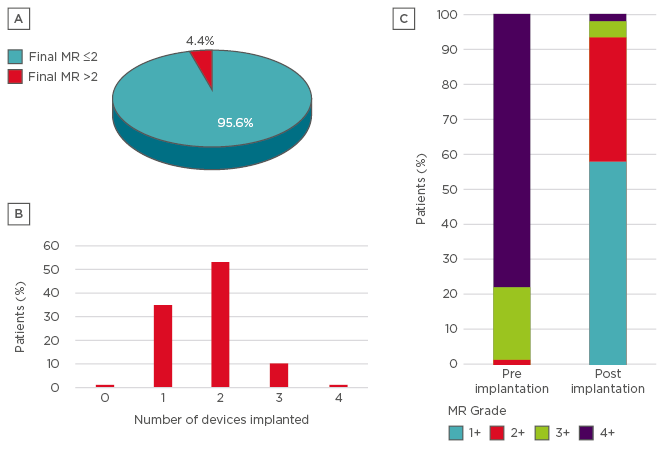
Figure 1: A) MitraClip® insertion procedural success: the number of patients who were discharged with a final mitral regurgitation graded ≤2; B) The number of MitraClip devices implanted in enrolled patients; C) Grading of mitral regurgitation pre and post device implantation.
MR: mitral regurgitation.
Periprocedural complications occurred in 37 patients (3.6%): 7 cases of cardiac tamponade, 1 transient ischaemic attack, 6 minor bleedings (5 due to haematoma at vascular access site), 8 partial clip detachments (3 requiring conversion to mitral valve surgery), 4 major bleedings, 1 case of major arrhythmia (ventricular fibrillation), and 1 myocardial infarction. The median duration of hospitalisation was 5 days (interquartile range: 3–7), with a median time of stay in the intensive care unit of 24 hours (interquartile range: 0.00–45.25). Most of the patients were discharged to their homes (83.9%), whereas 9.8% were sent to rehabilitation facilities, 2.4% to other wards, and 0.8% to non-cardiologic intensive care units.
The in-hospital mortality rate was 3.1% (32 deaths): 5 deaths were related to procedural complications, 25 were caused by multiorgan failure or cardiogenic shock despite procedural success, and procedural failures occurred in 2 cases. The main aetiology of the 25 patients who died in hospital despite procedural success was FMR (n=18, 72%), with a mean age of 77 years. A total of 23 of the 25 patients were NYHA Class III and IV; the mean ejection fraction was similar to survivors (39% versus 38%, respectively) but the mean systolic pulmonary artery pressure in the patients who died was higher (55 mmHg versus 46 mmHg, respectively). These acute results show the safety of the MitraClip procedure (3.1% 30-day mortality) with a high success rate (93.8% MR 2). Basic demographic and follow-up data will help to clarify the real impact of MitraClip in the management of MR and heart failure.








