Abstract
Bifurcation coronary lesions still represent a challenge for interventional cardiologists. Although provisional stenting is considered the gold standard for the treatment of bifurcations, some studies report good results with two-stent techniques. In the last few years, drug-coated balloons have been used for the treatment of several kinds of coronary lesion, such as in-stent restenosis, small vessels, and bifurcations. The use of drug coated balloons for the treatment of the side branch after provisional stenting is a promising option for further improving provisional stenting results.
INTRODUCTION
The treatment of coronary bifurcation lesions still represents one of the greatest challenges for interventional cardiologists, due to the technical complexity, the lower success rates compared to non-bifurcation lesions, and the lack of clear scientific data. In this review article, we will briefly describe the current treatment options for bifurcation lesions and examine more deeply the role of drug-coated balloons (DCB) in this context.
CORONARY BIFURCATION LESIONS
A coronary bifurcation lesion is defined as “coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant side branch”.1 A significant side branch (SB) is a branch that, if lost, can impact the prognosis of the patient; thus, determination of the SB as significant usually depends upon the subjective judgement of each single interventional cardiologist.
BIFURCATION CLASSIFICATION
Several different classifications of coronary bifurcation lesions have been proposed, due to the variety of possible bifurcation lesions, with different technical implications, treatment options, and prognoses. The most used, for its simplicity and reproducibility, is the Medina classification. This classification is based on the presence or absence of narrowing >50% on each of the three components of the bifurcation: the main branch proximal (MBP), the main branch distal, and the SB. A value of 0 or 1 is assigned to each of the three segments in the following order: MBP, main branch distal, and SB. For example, a bifurcation lesion involving the MBP and the SB would be defined as 1,0,1. Seven morphologies are therefore possible.2 Despite being the most used classification, the Medina has several limitations, since it does not consider the plaque burden, branch diameter, lesion length, bifurcation angles, the presence of ostial disease, or calcification. Thus, different classifications have been proposed, such as the Movahed classification.3,4
CURRENT TREATMENT OF BIFURCATION LESIONS
The goal of percutaneous coronary intervention in bifurcation lesions is to maximise flow in the main branch (MB), maintain flow in the SB, prevent its occlusion, and maximise long-term patency of both vessels. The provisional stent strategy is currently the standard approach for treatment of bifurcation lesions: it involves stenting the MB first (most commonly with a drug-eluting stent [DES]), and then evaluating whether there is a need to treat the SB (with balloon angioplasty or stenting), which would only be performed in cases of flow limitation, a large dissection, or a large myocardial territory subsiding the SB.5,6
When needed, stenting of the SB can be performed via a T-stenting technique, or with an overlapping technique, such as T and protrusion, culotte, or crush. At the end of the procedure, whether SB stenting has been performed or not, kissing balloon inflation (or post-dilation) can be performed, although its benefit is not clear.7
Despite being a valid approach, two-stent techniques are less frequently used, since the majority of studies have failed to demonstrate a benefit in choosing two-stent techniques over provisional stenting. A recent meta-analysis, including nine randomised trials comparing provisional strategy with two-stent techniques, demonstrated that a complex strategy has similar safety (death, stent thrombosis) and efficacy (restenosis, target lesion/ vessel revascularisation) compared to provisional stenting, despite carrying an increased risk of early and late myocardial infarction. However, subgroup analysis suggests that two-stent techniques may be preferable in patients with true bifurcation lesions (bifurcation with a lesion both in the MB and the SB), with large SB.8 Two-stent techniques include T-stenting (which is preferred for T-shape angulation), T and protrusion, culotte, and crush (which can be implemented with technical refinements, such as mini-crush, step-crush, or double kissing crush).9 The description of these techniques goes beyond the purpose of this review and thus will not be addressed.
The recent EBC TWO study comparing the provisional T-stent versus culotte two-stent technique in large caliber true bifurcation lesions, concluded that there is no difference between provisional strategy and a two-stent culotte strategy in a composite endpoint of death, myocardial infarction, and target vessel revascularisation at 12 months.10 Moreover, a recent analysis of 5-year survival from the NORDIC I and the BBC ONE studies demonstrated that 5-year mortality was lower among patients who underwent provisional stenting compared to a complex strategy (culotte, crush, and T-stenting).11 Finally, it is likely that double-stent strategies carry a higher risk of late stent thrombosis compared to single-stenting, as suggested by a meta-analysis of 12 major studies of bifurcation percutaneous coronary intervention, for a total of 6,961 patients.12
DRUG-COATED BALLOONS
DCB, on the other hand, have emerged as a possible alternative to DES to prevent restenosis. DCB are semi-compliant angioplasty balloons covered with an antiproliferative drug (most commonly paclitaxel, since sirolimus is not lipophilic) that is rapidly released upon contact with the vessel wall.13 DCB are not primarily used to improve the culprit stenosis; lesions should be pretreated with standard balloon angioplasty, a non-compliant balloon, and/or scoring balloons. When a good angiographic result is achieved, DCB can be inflated for 30–90 seconds, depending on the DCB used, to allow adequate drug transfer.
DCB thus combine mechanical expansion of the vessel and reduction of neo-intimal hyperplasia without leaving a foreign body, abolishing the risk of late and very late stent thrombosis and reducing the need for dual antiplatelet treatment.14 Currently, the use of DCB is established in the treatment of in-stent restenosis (ISR), as first described in the PACCOCATH ISR I trial.15 Further studies have confirmed the superiority of DCB in the treatment of bare-metal stent (BMS) ISR over a paclitaxel-eluting stent, also at long-term follow-up.16
In regard to DES ISR, the role of drug-eluting balloons (DEB) is more controversial; DCB have proven to be superior to plain old balloon angioplasty (POBA) for the treatment of ISR occurring in a previously implanted DES in the PEPCAD-DES trial.17 Furthermore, the ISAR-DESIRE 3 trial compared DCB with paclitaxel-eluting stents in DES ISR and showed no differences between groups in the frequency of death, myocardial infarction, or target lesion thrombosis.18 On the other hand, DCB have not proven to be superior compared with newer DES: the RIBS V trial compared the DCB with a second-generation DES (everolimus-eluting stent) in the treatment of BMS ISR; at 9 months, the DES group had superior clinical outcomes, including reduced need for target lesion revascularisation (TLR) (8% versus 16%).19
However, it is important to underline that not many studies have been conducted in this context. A meta-analysis of observational and randomised data, comparing outcomes in the management of DES ISR using DES, DCB, or POBA showed that the relative risk reduction for TLR for DES was similar to DCB but without the need for an additional stent layer.20 All being said, as depicted by European Society of Cardiology (ESC) Guidelines on myocardial revascularisation, DCB are recommended for the treatment of ISR after prior BMS or DES, with a Class I indication and level of evidence A.21
Another application for DCB is the treatment of small-vessel disease, when technical difficulties outweigh the benefit of placing a stent and where there is more neo-intimal hyperplasia and therefore a higher risk of restenosis.22 Numerous studies, including the BELLO trial, described a benefit in using DEB instead of placing a stent in vessels with a diameter <2.5 mm.23
DRUG-COATED BALLOONS IN BIFURCATION LESIONS
As previously outlined, the treatment of bifurcation lesions is controversial and carries numerous technical difficulties. As previously reported, provisional stenting strategy is the preferred technique for bifurcations; therefore, DCB could carry a potential benefit by administrating an anti-proliferative drug to the vessel wall without stenting the SB. Deploying a stent in the SB could lead to inadequate expansion at the ostium or the protrusion of stent struts into the MB, carrying increased rates of complications without the provision of long-term benefits. As a matter of fact, the incidence of TLR ranges between 1.3% and 17.9%, depending on the population and the technique used. The incidence of stent thrombosis is between 0.4% and 3.7% at 1 year.24 On the other hand, suboptimal SB results may carry negative prognostic implications.25 Moreover, SB restenosis may range between 7.9% and 15.4%.26
Recent studies have been conducted to evaluate if DCB could be beneficial in the treatment of coronary bifurcation lesions, considering the benefit in ISR and in small vessel disease (Table 1). The PEPCAD V registry was a prospective, multicentre, single-arm trial, in which 28 patients were treated with pre-dilation using a DCB in both the MB and the SB, followed by BMS implantation on the MB only when thrombolysis in myocardial infarction flow was <2, or the MB had a stenosis >50% (14.3% of patients). In this study, the procedural success was 100%. At 9 months, the reported restenosis rate was only 3.8% in the MB and 7.7% in the SB and this was lower compared to restenosis after DES implantation in other studies (4.6–6.7% [MB] and 13.2–14.7% [SB] in the CACTUS study; 0.6–5.1% [MB] and 11.5–19.2% [SB] in the Nordic study).27-29
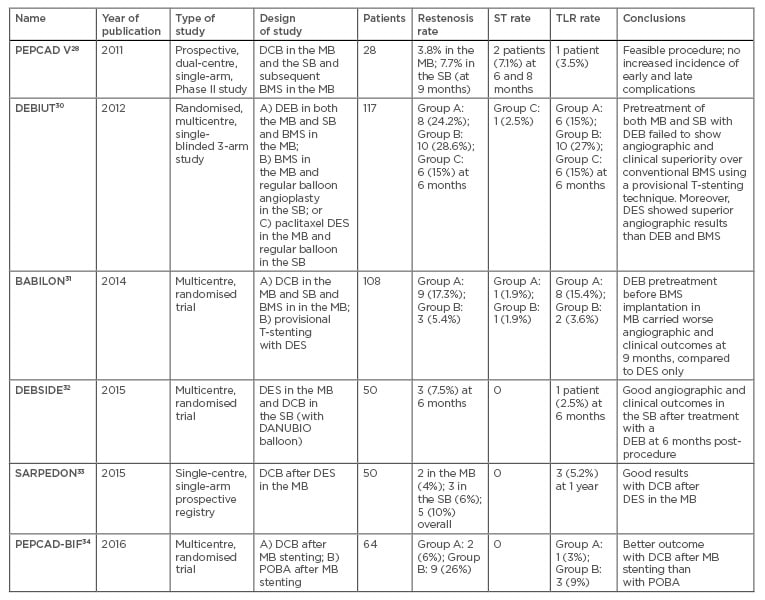
Table 1: Studies of drug-coated balloons in bifurcation lesions.
TLR: target lesion revascularisation; ST: stent thrombosis; DCB: drug-coated balloon; MB: main branch; SB: side branch; BMS: bare-metal stent; POBA: plain old balloon angioplasty; DES: drug-eluting stent.
The 2012 multicentre, randomised DEBIUT trial compared three different strategies among 117 patients: DCB in both the MB and SB and BMS in the MB; BMS in the MB and POBA in the SB; paclitaxel DES in the MB and regular balloon in the SB. This study showed that angiographic outcome was similar in the group with DCB+BMS compared with BMS only, but inferior to the group with DES in the MB, suggesting that pretreatment with DCB did not carry any advantage over DES. However, binary restenosis rates at 6 months and major adverse cardiovascular event (MACE) rates were similar between the three groups at 12 months.30 Negative results came also from the BABILON trial, in which DEB pretreatment before BMS implantation in the MB carried worse angiographic and clinical outcomes at 9 months, compared to DES only.31
On the other hand, the DEBSIDE trial analysed the role of DCB in the SB, using the novel DANUBIO balloon, after placement of a DES in the MB; in this group of 52 patients, the results were promising, with a very low risk of complications and of TLR (1 patient) at 6 months, with a good angiographic outcome.32 Similar results were found in the SARPEDON study which assessed the efficacy of DCB at the SB ostium after DES implantation in the MB, with good angiographic outcome and low rate of restenosis, although a high rate of MACE (19% at 1 year).33
Finally, the PEPCAD-BIF multicentre trial was published in 2016, which enrolled 64 patients with a bifurcation lesion and randomised them to DCB versus POBA after MB stenting. Only 5 patients underwent stenting in the SB as a bail-out strategy. The trial showed that the use of DCB after MB stenting was superior to POBA for restenosis rate (6% versus 26% in the POBA group; p=0.045), TLR (1 patient versus 3 patients) and angiographic endpoint.34
CONCLUSIONS
Despite the lack of data, the use of DCB in the treatment of bifurcation lesions in addition to standard provisional stenting could be an innovative and useful strategy when SB stenting is not needed, because of the lack of additional procedural risk compared to standard treatment and because of the possible positive prognostic implications, especially by reducing the risk of progression of the disease within the SB.
In our opinion, DCB could be an option for the treatment of the SB after provisional stenting of the MB with a new-generation DES. Further studies are needed to determine whether DCB could improve the overall treatment of bifurcation lesions, since current data is not sufficient to establish the correct treatment for bifurcations lesions and for the use of DCB in this context.








