Abstract
Background: Surgical site infections (SSI) remain a major cause of hospital-acquired infections, causing morbidity and mortality worldwide. In developing countries, 5.6% of surgical procedures will develop SSIs. These are further complicated by an increasing prevalence of multidrug-resistant organisms. Associated risk factors also play a role in contribution of SSIs. However, the identification of factors that cause or predict these SSIs remains an important area of research.
Objective: To investigate the risk factors for SSI together with the identification of the aetiological bacterial agents and their antimicrobial susceptibility.
Methods and Patients: A cross-sectional study was carried out on 143 patients who underwent surgery in a single tertiary care centre. Only the surgeries falling under clean and clean-contaminated categories were included in the study. SSI was determined by positive bacterial culture, and resistant pattern was determined by Kirby–Bauer disc diffusion method.
Results: Out of 25 different surgical procedures in 143 cases, four cases developed SSI due to Escherichia coli and Staphylococcus aureus. Diabetes, obesity, and smoking were the associated risk factors in these cases.
Conclusion: Prevention of SSI is complex and requires the integration of a range of preventive measures before, during, and after surgery.
Key Points
1. Surgical site infections (SSI) are a major cause of morbidity and mortality worldwide. These are further complicated by an increasing prevalence of multidrug resistant organisms, leading to increased average length of hospital stay among patients with SSI, which causes increased financial implications.
2. Patients with associated risk factors are at higher chances of developing SSIs. Modifiable patient factors such as glycaemic control in diabetes, managing hypertension, and ceasing of nicotine for weeks prior to surgery facilitates prevention of SSI and betters the management of patients.
3. Determining the antimicrobial patterns of the bacterial agents causing SSIs will help institutions to improve antibiotic policy and restrict the use of antimicrobials in preventing the spread of drug resistance in hospitals, which is needed as a part of antimicrobial stewardship.
INTRODUCTION
Surgical site infections (SSI) are a leading cause of morbidity and mortality around the world. Around 5.6% of surgical procedures develop SSIs, mostly in developing countries.1 To track healthcare-associated infections, the National Healthcare Safety Network (NHSN) uses standardised infection ratio, which compares the number of observed infections with the number of predicted infections.2
Each year, a significant amount of morbidity and mortality is caused by infection at or around the surgical site, which occurs within 30–90 days of an operative procedure.3 A Centers for Disease Control and Prevention (CDC) survey from 2015 estimated approximately 110,800 SSIs among inpatient surgeries.4 There was 5% reduction in SSIs in 2020 when compared with 2015 data as baseline among all NHSN operative procedure categories combined.5
Despite improvements in surgical techniques, sterilisation of instruments, operation theatre practices, and the best efforts of infection prevention strategies, SSIs remain a major cause of hospital-acquired infections.6 These are further complicated by an increasing prevalence of multidrug-resistant organisms.
Most of the time, it is the patient’s endogenous flora that is responsible for many SSIs, and the commonly isolated pathogens include Staphylococcus aureus, coagulase-negative staphylococci, Enterococcus spp., and Escherichia coli.7
However, the identification of factors that cause or predict these SSIs remains an important area of research. The authors aim to investigate the risk factors for SSIs, together with the identification of the aetiological bacterial agents and their antimicrobial susceptibility in a tertiary hospital.
METHOD AND PATIENTS
A cross-sectional study was carried out on 143 patients who underwent surgery in a single tertiary care centre. The study was conducted over a period of 2 months between August–September 2021. The degree of surgical wound contamination was assessed by the operating team at the time of surgical procedure. The wounds were classified into clean, clean-contaminated, contaminated, and dirty/infected, based on NHSN wound classifications.8 The study included patients who underwent elective surgeries falling under clean and clean-contaminated cases with at least 7 days of hospital stay post-operatively, and who experienced signs and symptoms such as redness, pain, swelling around the surgical site, tenderness over the site, fever, delayed healing, etc. A written informed consent was obtained from the patients who agreed to participate in the study. Wounds falling under the categories of contaminated and dirty/infected were excluded from the study. Data was collected using a specially designed case report form.
Sample Collection and Processing of Specimens
Two swabs were collected from the surgical site taking aseptic precautions, and transported immediately to the laboratory in a sterile container to be added. One swab was subjected to Gram stain, for the presence of pus cells and organisms. Another swab was cultured on blood agar media, MacConkey agar media, and Thioglycolate broth. Interpretation of the cultures and identification of the organisms was done as per standard protocol, and antibiotic sensitivity was done using Kirby–Bauer disc diffusion method. Sensitivity pattern of the isolates are recorded as per Clinical and Laboratory Standard Institute (CLSI) guidelines.9 Institutional Ethical Committee approval (letter number: RRMCH-IEC/77/2021; dated: 29.07.2021) was obtained for this particular study before commencing the study.
STATISTICAL ANALYSIS
Demographic variables were summarised using means for continuous variables. To know the significant difference between risk factor and presence or absence of SSI, analyses were done using the Z-test. A p value of <0.05 was considered statistically significant.
RESULTS
A total of 481 cases were admitted for surgery during the study period. Of these, 338 cases were excluded from the study group as the wound belonged to contaminated or dirty/infected classification.
A total of 143 cases were included in the study as per inclusion criteria (Figure 1) The mean patient age ranged from 15–75 years; however, the majority (81.8%) of the study group were aged between 35–65 years. The majority of the patients were male (76%). Out of 143 cases, 79 (55.2%) had patient-related risk factors, and 64 (44.8%) cases did not have associated risk factors. Among the study group, 36.4% had uncontrolled diabetes, 17.8% had obesity, 10.2% were smokers, and 7.6% had associated hypertension (Figure 2).
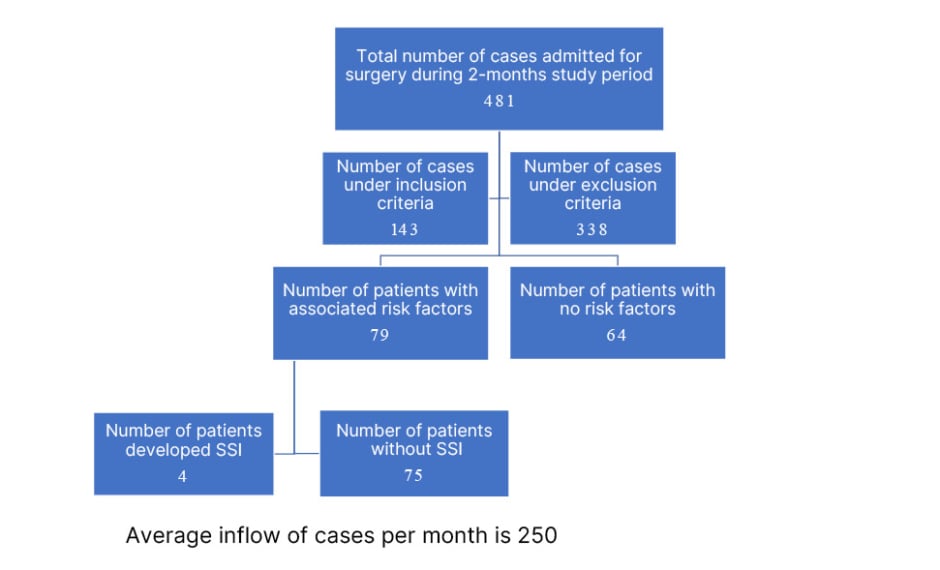
Figure 1: Flowchart depicting study methodology.
SSI: surgical site infection.
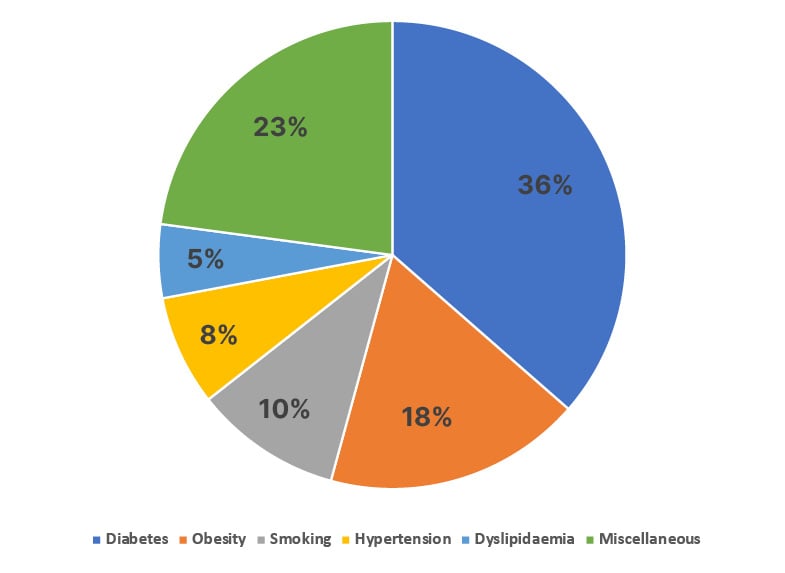
Figure 2: Surgical cases with associated risk factors.
Out of 79 cases with risk factors, four (5.06%) patients developed SSI. These four patients had diabetes with history of tobacco chewing, diabetes with chronic cough, and diabetes with obesity, and hypertension, respectively, as an associated risk factor. A significant result with p<0.05 was noted when analysis was done for the presence of risk factors, and their association with SSI, using Z-test for proportion (Table 1)
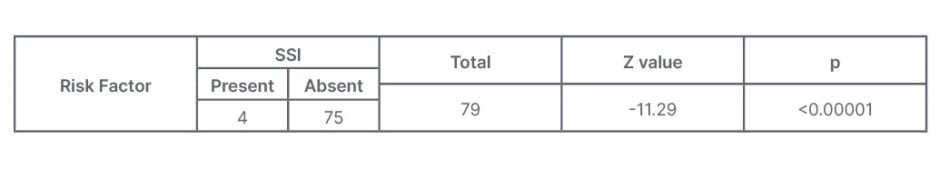
Table 1: Analysis using Z-test for proportion of risk factor present, associated with surgical site infection.
SSI: surgical site infection.
A total of 25 different surgical procedures were done under clean and contaminated wound category on 143 cases during the study period. Of these, nine cases showed symptoms of redness and discharge at the site of incision. Wound swabs collected showed culture positive in four (2.8%) cases. These cases had undergone hernioplasty, mastectomy, lower segment Caesarean section, fenestration, and discectomy surgeries, respectively. Out of four positive cultures, E. coli was isolated from two patients (2.5%) and S. aureus in the other two cases (2.5%). Out of the two strains of S. aureus one was Methicillin-resistant S. aureus. Antibiotic susceptibility pattern of E. coli isolates showed resistance to ampicillin (100%), β-lactams (50%), cephalosporins (50%), and ciprofloxacin (50%), and were sensitive to aminoglycosides (100%) and carbapenems (100%). Both isolates of S. aureus were sensitive to linezolid, vancomycin, and clindamycin (100%). A case-wise SSI summary is shown in Table 2.
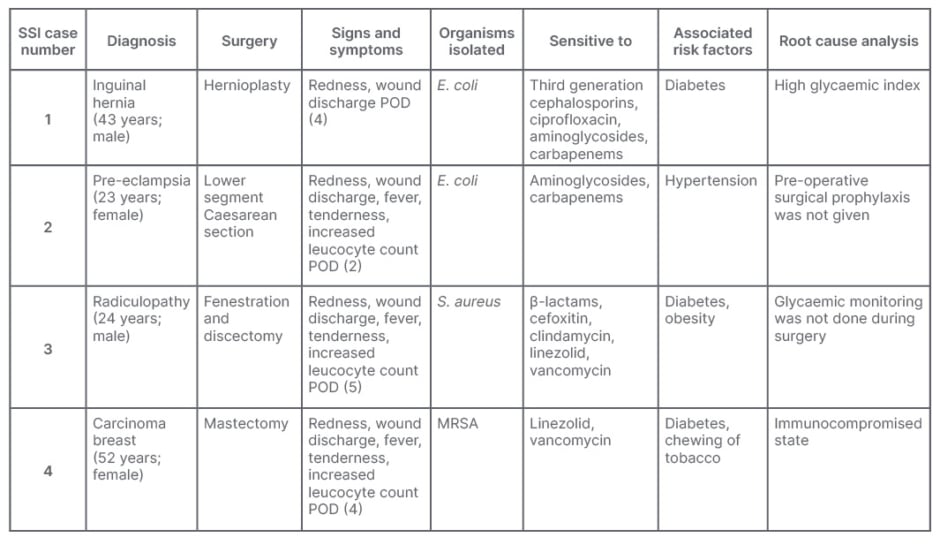
Table 2: Case-wise surgical site infection summary.
E. coli: Escherichia coli; MRSA: methicillin-resistant Staphylococcus aureus; POD: post-operative day;
S. aureus: Staphylococcus aureus; SSI: surgical site infection.
All SSI cases were treated with appropriate antibiotic coverage and subsequently discharged home after wound healing and without any further complication.
DISCUSSION
SSIs are the infections that occur following a surgery at surgical site within 30–90 days of surgical procedure. Infection could be superficial, involving skin and subcutaneous tissue, or a serious infection involving deeper tissues, organs, or the implant itself.10 In low-and middle-income countries, SSIs are the most surveyed and most common type of infection, with incidence rates ranging from 1.2–23.6 per 100 surgical procedures.11
Several studies from India have reported SSI rates ranging from 0.04–22.00%.12,13 The authors’ study reported 2.8% of SSIs, which is similar to a study by Satyanarayana et al.14 SSIs are a major cause of morbidity and mortality worldwide, affecting 5.6% of surgical procedures, mostly in developing countries.1
Mangram et al.15 have demonstrated several patient characteristics like diabetes, smoking, obesity, and remote site infections to have a significant, independent association for SSI prediction. A systemic review and meta-analysis by Martin et al.16 reported significant association between diabetes and SSI that was consistent across multiple types of surgeries. Similar association was noted in the authors’ study, where three out of four patients who had developed SSI had diabetes.
As the number and complexity of surgical procedures performed today are increasing, so does the cost of human life and financial burden if a person develops SSI, especially if there are associated comorbidities.17-19 Numerous studies have proven increased financial implications and increased average length of hospital stay among patients with SSI when compared to non-infected patients with similar surgeries. 3,20-22
In the present study, SSIs were recorded in the age group 22–65 years, which was also seen in the similar study by Keith et al.23 However, gender was not a significant factor for prediction of SSI risk in the authors’ study, which is similar to study by Berard et al.24
In the majority of SSIs, infections are mainly because of patients’ endogenous flora. The aetiological agents will also depend on the type and location of the surgery. Various studies have reported E. coli and S. aureus as the frequent microbial flora associated with SSI, similar to the authors’ study.25,26
In a hospital setting, various factors like poor infection control practices, inadequate sanitary conditions, and irrational use of antibiotics will favour development and spread of antimicrobial resistance. Hence, understanding the sensitivity pattern of the causative agent is crucial to initiate appropriate treatment. In the present study, E. coli was found to be 100% sensitive to aminoglycosides and carbapenems. S. aureus was sensitive to linezolid, vancomycin, and clindamycin (100%), which is comparable to studies by Mundhada et al.22 and Dessie et al.27
High rates of methicillin-resistant S. aureus in clinical isolates from various studies in India have been documented, with rates as high as 41% reported.28 In the authors’ study, one of the two isolates of S. aureus was methicillin resistant.
Various factors influence the incidence of SSIs, such as pre-operative care, environment of operation theatre, efficient central sterile supply department, post-operative care, type of surgery, and associated host factors. Along with that, the factors that influence surgical wound healing and determine the potential for infection also play a vital role.
Numerous studies have estimated that approximately 60% of SSIs can be prevented by using evidence-based guidelines.29,30 Berríos-Torres et al.31 have recommended pre-operative full body bath; surgical prophylaxis as per clinical practice guidelines; surgical site skin preparation using alcohol-based agent; maintaining glycaemic levels less than 200 mg/dL; maintaining normothermia; and administration of increased fraction of inspired oxygen during surgery and after extubation in a patient undergoing surgery under general anaesthesia with endotracheal intubation and administration of blood products if required for preventing SSI. These guidelines can be incorporated into quality improvement programmes to have an holistic approach in prevention of SSIs and to improve patient safety.
In this regard, it is important that with multidisciplinary approaches and available preventive guidelines, improved antibiotic policy and addressing modifiable patient comorbidities before, during, and after surgery will help in prevention of SSI. Determining the antimicrobial patterns of the bacterial agents causing SSIs will help institutions to improvise antibiotic policy, and restrict the use of antimicrobials in preventing the spread of drug resistance in a hospital.
LIMITATION
The human behaviours in the form of hand hygiene and other complex nature of factors involved in development of SSI are the limitation of this study.
CONCLUSION
This study demonstrates significant association between patient-related risk factors and the development of SSIs.
Modifiable patient factors in the form of glycaemic control in diabetes, managing hypertension, and cessation of nicotine for weeks prior to surgery will facilitate the prevention of SSIs, which will assist in better management of surgical cases by reducing the length of stay in the hospital, and thereby reduce financial burden following surgery.
The early identification of SSI, supplemented with microbial cultures, will aid in initiation of early treatment with appropriate antibiotics, which will further prevent emergence of multidrug-resistant strains.







