Abstract
Introduction: The objectives of this retrospective study were to describe clinical presentations and mortality outcomes of hospitalised patients with the COVID-19 Omicron variant within two acute district general hospitals, and to evaluate demographic factors associated with these presentations and mortality.
Methods: Data was obtained over a month in 2021–2022 from multi-ethnic patients who were hospitalised and detected to have severe acute respiratory syndrome coronavirus 2 Omicron infection. Details included socio-demographic characteristics, vaccination, and mortality. Patients were subdivided into three groups: Group 1 were admitted with true COVID-19 pneumonitis, Group 2 had incidental COVID-19 on admission screening, and Group 3 were negative on admission but developed COVID-19 over 7 days post-admission.
Results: Of 553 patients, only 24.1% (133/553) were in Group 1, 58.2% (322/553) in Group 2, and 17.7% (98/553) in Group 3. Patients in Group 1 and Group 3 were significantly older than those in Group 2 (p<0.001). Thirty percent of patients from Black, Asian, and minority ethnic backgrounds had COVID-19 pneumonitis compared with 19% of those with White ethnicity (p=0.002). Twenty percent of patients were admitted within nonmedical specialties, i.e., surgical specialties, paediatrics, and obstetrics. Of 36 requiring critical care, 21 were in Group 1. Of those patients, 20/21 (95%) were unvaccinated and seven of the 21 who died were all unvaccinated (100%). Common COVID-19 presentations included delirium, falls, seizures, chronic obstructive pulmonary disease, and antenatal problems. Overall, 13.7% (76/553) patients died and 4.7% (26/553) were directly attributable to COVID-19.
Conclusions: This large, multi-ethnic study has described clinical presentations and mortality of hospitalised patients with Omicron. It has determined socio-demographic factors associated with these presentations, including ethnicity and vaccination rates. The study provides useful information for future COVID-19 studies examining outcomes and presentations of Omicron and future COVID-19 variants.
Key Points
1. This is one of the first large, multi-ethnic, hospital-based studies that has described the clinical presentation of hospitalised patients with Omicron COVID-19 infections. Unlike previous surges in the UK, there were significantly fewer patients admitted with true COVID pneumonitis (24%). While 58% were admitted for other reasons and had COVID-19 detected on routine admission screening, 18% patients had probable hospital-associated COVID-19 infections.
2. Patients with COVID-19 from Black, Asian, and minority ethnic backgrounds had significantly higher rates of COVID-19 pneumonitis (30%) compared with those from White ethnicity (19%).
3. The authors’ findings are consistent with other recent studies, which also found that Omicron infections caused less severe illness and death, and that many deaths that may be classified as COVID-19-related were actually not directly attributable to COVID-19 pneumonitis.
INTRODUCTION
Since the detection of the first cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant causing COVID-19 infections in South Africa in November 2021, there have been a few population-based reports to suggest that the clinical severity and presentation of this variant is different to previous COVID-19 surges.1-4 This variant is known to have several mutations to previous variants of this virus; hence, it was predicted to be much more infectious due to possible immune evasion.5
Population-based reports have evaluated clinical severity of Omicron COVID-19 in the general population.4 There are few studies that have examined the demographic and clinical presentation of hospitalised patients with Omicron COVID-19 infections.6,7 A recent South African study described the clinical presentation of hospitalised patients with the Omicron variant, but that study did not differentiate between those patients admitted with symptoms of COVID-19 infection from those who were admitted for other reasons, or were already in hospital and were found to have an incidental positive COVID-19 test result.7 A recent study showed that the outcomes of the presumed Omicron variant were substantially better than previous variants, but the study did not describe the clinical presentations and socio-demographic associations of these patients.8
The objectives of this retrospective, observational study were to describe the clinical presentations and mortality outcomes of hospitalised patients with the COVID-19 Omicron variant within a busy acute district general hospital trust, and to evaluate demographic factors associated with these presentations and mortality.
METHODS
Data was obtained from a retrospective survey of all patients hospitalised in an acute London, UK, hospital trust who were detected to have SARS-CoV-2 Omicron variant infection over a month from 15th December 2021 to 15th January 2022. The trust provides healthcare to a diverse, multi-ethnic, inner-city population from two extremely busy acute district general hospital legacy sites. Whilst information on precise genotype of the COVID-19 variant was not available, national data had shown that 87.5% of COVID-19 infections within London were due to the Omicron variant by 15th December 2021.9
Since mid-2020, the hospital trust has a policy of screening every hospital admission for COVID-19; therefore, on admission, all patients undergo an urgent routine PCR test to screen for COVID-19 infection. Panther® Fusion SARS-CoV-2 assays (Hologic, Marlborough, Massachusetts, USA) were employed for this test.10 This is a real-time, reverse transcription PCR, in vitro diagnostic test intended for the qualitative detection of SARS-CoV-2 RNA, isolated and purified from nasopharyngeal and oropharyngeal swab specimens.10
For this study, data was obtained from the hospital electronics patient record system. Data included socio-demographic details such as age, sex, and ethnicity. Clinical data included presenting complaints (reasons for admission), COVID-19 vaccination status, whether critical care support was required, admitting specialty, and mortality outcome.
These patients were divided into three groups for analyses. Group 1 included those patients who were admitted with COVID-19 pneumonitis (true COVID-19). For the purpose of this study, the pragmatic definition of this diagnosis was based on the presenting clinical signs and symptoms of the patient, as stated by the admitted medical team and confirmed by the admitting consultant. Group 2 included patients who were admitted for a different reason to COVID-19 pneumonitis, but their routine PCR COVID-19 screening test on admission was positive (incidental COVID-19). Group 3 included those patients who were negative for COVID-19 on admission but developed the infection more than 7 days after admission i.e., probable hospital-associated COVID-19 (HAC) infection.
Simple descriptive statistical methods were used to examine the prevalence rates of the antibodies within various socio-demographic groups. Simple statistical χ2 tests of distribution were performed using Stata statistical package (StataCorp, College Station, Texas, USA). Multivariable analyses, using stepwise backward logistic regression, were also conducted to identify any independent differences between the three designated groups. It was not appropriate or possible to involve patients or the public in the design, conduct, reporting, or dissemination plans of the research.
RESULTS
There were 553 patients hospitalised in the trust that were detected as having COVID-19 infection between 15th December 2021 and 15th January 2022. Unlike the previous two surges in the UK, there were significantly fewer patients admitted with true COVID-19 pneumonitis; therefore, Group 1 only included 24.1% (133/553) of patients. Group 2, which included patients who were admitted for other reasons and had COVID-19 detected on routine admission screening, included 58.2% (322/553) of participants. Finally, Group 3, which was made up of patients who had probable HAC, included 17.7% (98/553) of participants.
The data was analysed for all patients in the survey, as well as the three groups individually, according to various socio-demographic factors (Table 1). As might be expected, patients with COVID-19 pneumonitis (Group 1) and HAC (Group 3) were significantly older than those in Group 2. However, there were no significant differences across the three groups in terms of sex.
The distribution of clinical presentation in terms of ethnicity showed that there was a significantly greater proportion of White patients in Group 3. A greater proportion of older, frail patients who are in hospital for a longer period were more likely to be of White ethnicity. While the distribution of other ethnic groups appeared similar across Groups 1 and 2, it is interesting to note that 30% (36/120) of Black Caribbean, 25% (17/67) of Black African, and 36% (14/39) of South Asian patients had COVID-19 pneumonitis compared with 19% (62/319) of patients from White ethnicity. Thus, 30% (71/234) of patients from Black, Asian, and minority ethnic (BAME) backgrounds had COVID-19 pneumonitis, which was significantly higher than patients of White ethnicity (19% [62/319]; p=0.002).
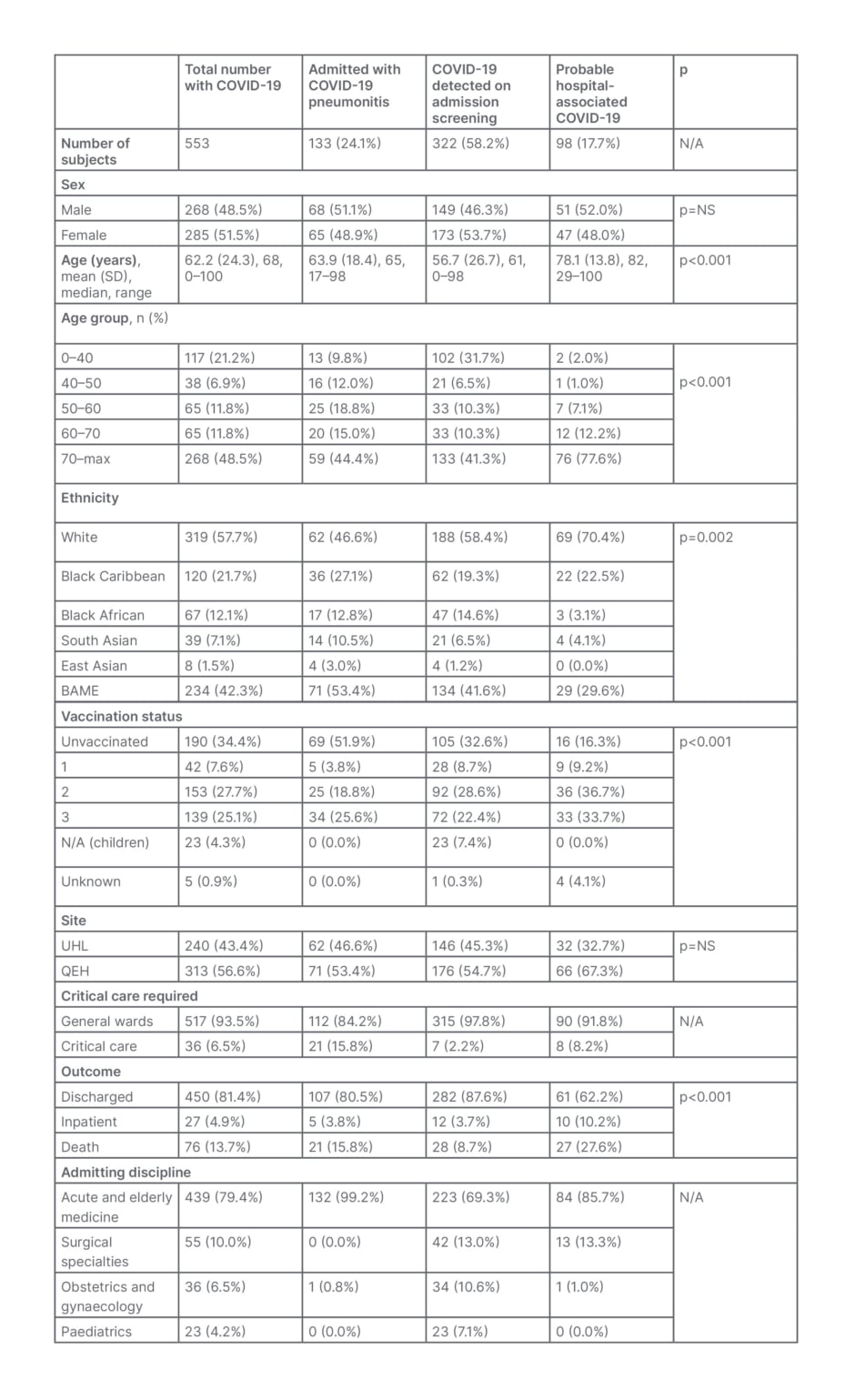
Table 1: Hospitalised patients with COVID-19 (Omicron) at Lewisham and Greenwich Trust, London, UK, from 15th December 2021 to 15th January 2022.
BAME: Black, Asian, and minority ethnic; N/A: not applicable; NS: not significant; QEH: Queen Elizabeth Hospital; SD: standard deviation; UHL: University Hospital Lewisham.
Multivariable analyses, using stepwise, backward, logistic regression and controlling for age, sex, and ethnicity, showed that older age >70 years (odds ratio [OR]: 2.4; 95% confidence interval [CI]: 1.2–4.5) and being South Asian (OR: 2.1; 95% CI: 1.1–4.3) were independently associated with COVID-19 pneumonitis.
Unlike the previous two surges, 20.7% of patients with COVID-19 were admitted within nonmedical specialties, i.e., surgical specialties, paediatric medicine, and obstetrics. Fewer patients required critical care support compared with previous surges. Of 36 patients requiring this support, only 21 were admitted due to COVID-19 pneumonitis. Ninety-five percent (20/21) of these patients were unvaccinated; seven of the 21 who died were all unvaccinated.
Of those admitted with COVID-19 pneumonitis, 52.0% (69/133) were unvaccinated, and a further 22.5% had had only one or two vaccinations. Thus, only 25.0% of those admitted with COVID-19 had triple vaccinations. Similar rates were observed in Group 2 as well. In Group 3, 75% of patients had between two and three vaccinations.
Table 2 describes the top presentations of those patients in Group 2. Unlike the previous surges when the presenting complaint for hospitalised patients was almost exclusively COVID-19 pneumonitis, this study showed that common presentations, including delirium, falls (some leading to significant fractures), seizures, and acute exacerbations of chronic obstructive airways disease or asthma, were associated with co-existing COVID-19 infection. COVID-19 was detected in patients admitted for antenatal problems.
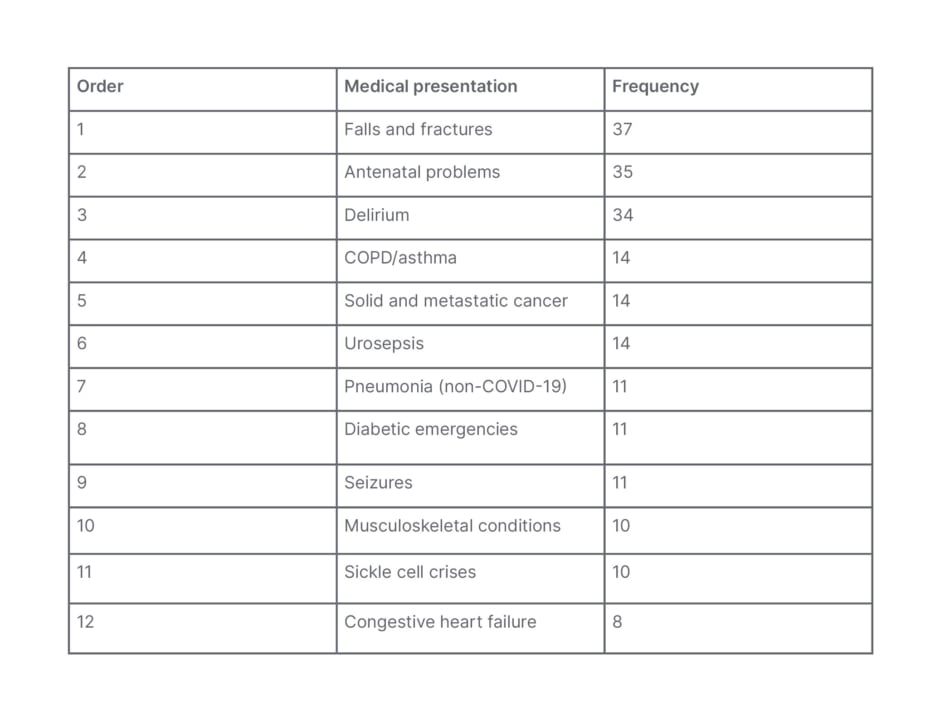
Table 2: Top 12 presentations of patients admitted with incidental Omicron COVID-19.
COPD: chronic obstructive pulmonary disease.
This study also described the mortality rates post-COVID-19 (Tables 1 and 3). In total, 13.7% of patients with COVID-19 died. For those with true COVID-19 (Group 1), the rate was 15.8%. Of the 76 deaths, only 21 were admitted with COVID-19 pneumonitis (27.6%).
Further analyses of patients who died in this study showed that of those who were not admitted with COVID-19 pneumonitis (Group 2), only 7/322 (2.2%) went on to develop COVID-19 pneumonitis and of these, only one died due to COVID-19. Similarly, in Group 3, 6/98 (6.1%) developed COVID-19, of whom four (4.1%) died. All five patients who died in Groups 2 and 3 had multiple comorbidities. Of the 55 deaths in Groups 2 and 3, only five had developed COVID-19 pneumonitis before their death. There were, therefore, 26 deaths directly attributable to COVID-19 pneumonitis. This represents only 4.7% (26/553) of all patients admitted with COVID-19. Of these 26 deaths, only six patients had had triple vaccinations, 11 patients were unvaccinated, and nine had between one and two vaccinations. Admittedly, the numbers are small for any meaningful comparisons.
Multivariable analyses, using stepwise, backward, logistic regression, showed that people from a Black Caribbean background (OR: 0.27; 95% CI: 0.07–0.98) were independently associated with lesser mortality, controlling for age, sex, and ethnicity.
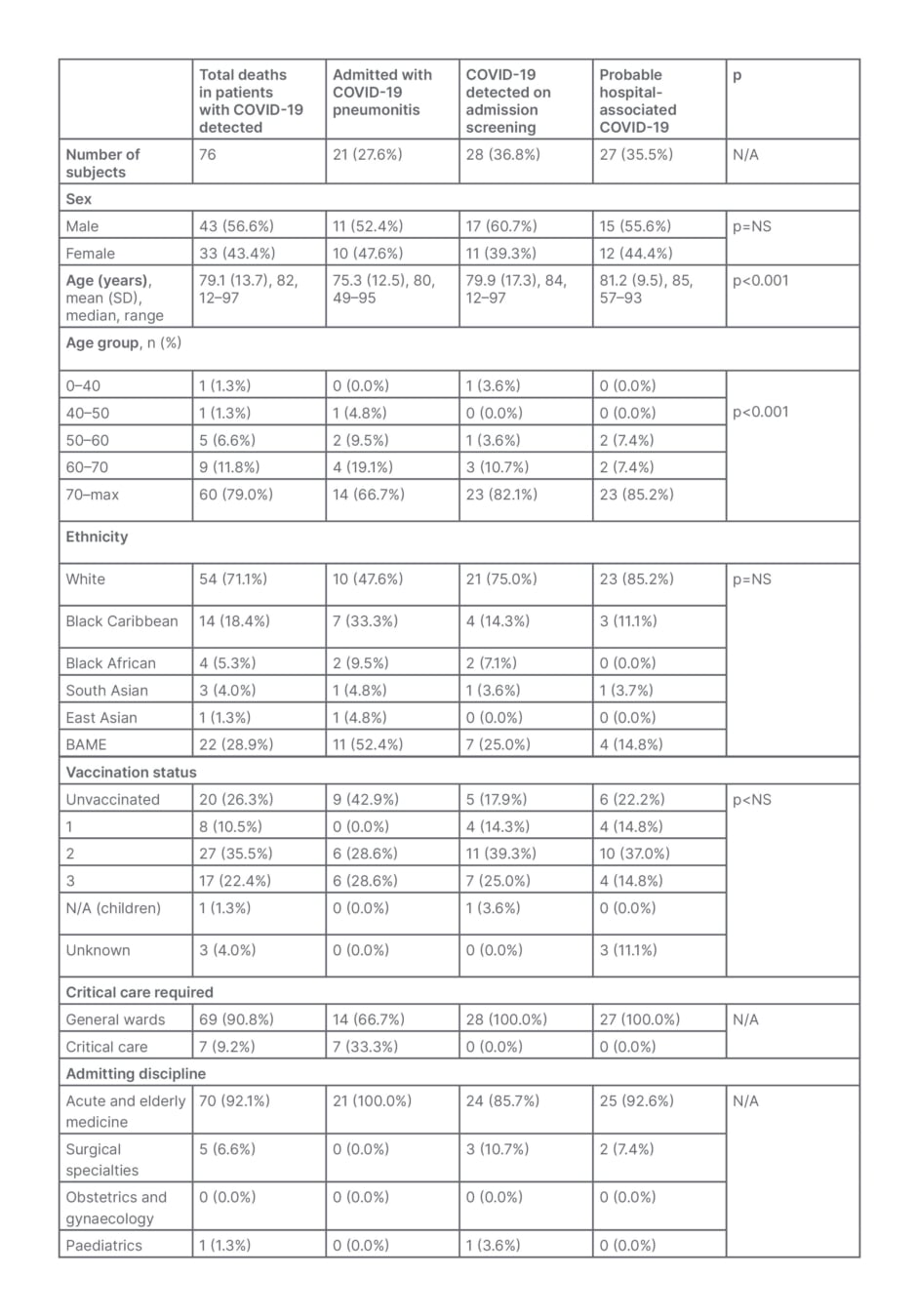
Table 3: Mortality in patients with COVID-19 (Omicron) at Lewisham and Greenwich Trust, London, UK from 15th December 2021 to 15th January 2022.
BAME: Black, Asian, and minority ethnic; N/A: not applicable; NS: not significant; SD: standard deviation.
DISCUSSION
This is one of the first large, multi-ethnic, hospital-based studies that has described the clinical presentation of patients hospitalised with Omicron COVID-19 infections and showed that these presentations are very different to those who presented to hospital in the previous surges in the UK. There have been very few studies that have described the clinical characteristics of patients hospitalised with the Omicron variant of COVID-19.7,8 A recent South African study showed that patients admitted due to the Omicron variant had significantly lower odds of severe disease compared with the Delta variant (OR: 0.3; 95% CI: 0.2–0.5), but that study did not describe the actual clinical presentations.7
The strengths of this study include the large number of patients managed within a very short period of time, thereby giving a good indication of proportion of the disease within the three designated groups of this study; multi-ethnic diversity of the cohort, which implies the rates could be generalisable to other healthcare populations; the study’s ability to examine various socio-demographic factors associated with the prevalence of the infection, which would enable healthcare institutions in terms of future healthcare planning; detailed information on the presenting clinical features of these patients confirming that Omicron COVID-19 is significantly different in its presentation and pattern compared to previous COVID-19 variants; and the novel socio-demographic and outcome comparison between the three groups identified in this study.
This study showed that a significant proportion of patients presented to hospital with other symptoms and conditions, and that they had an incidental positive COVID-19 test result on admission screening for COVID-19. Common presentations included delirium, falls and fractures, and non-COVID-19 respiratory illnesses (Table 2). These are recognised common presentations in hospitalised older adult patients; therefore this observation is reflective of the fact that most COVID-19 admissions to hospitals are amongst older, frailer patients with existing comorbidities. Furthermore, this study showed that COVID-19 was also incidentally detected in the maternity units among females presenting with antenatal problems, in a variety of surgical specialties, and in children. Seizures were the most common presenting feature in children. These observations are valuable for clinicians managing patients in various hospital specialties and would have implications in infection prevention and control, and in-hospital clinical pathways in terms of COVID-19 and non-COVID-19 pathways.
The authors also examined socio-demographic associations of hospitalised patients with COVID-19. They found that patients with COVID-19 pneumonitis (Group 1) and HAC (Group 3) were significantly older than those in Group 2. These differences could be explained to a certain extent by the fact that Group 2 had patients who were children or who had antenatal problems. Both of these cohorts included younger patients than those with other presentations. In accordance with previous studies, 30% of BAME patients had COVID-19 pneumonitis, which was significantly higher than 19% of patients from White ethnicity. There are possible speculative hypotheses that may explain these differences, including ethnic genetic variability in terms of innate immune response to viral infections, though yet unproven in COVID-19 infection specifically;11,12 higher prevalence of underlying health diseases such as diabetes, which may lend them to be more susceptible to developing infections;13-16 and worse deprivation rates and higher household density amongst BAME population.13,15-17 While there was no data available for the authors’ study on whether the Delta variant was more prevalent in patients from BAME backgrounds compared with White patients, they do not believe that there were any ethnic variations in the prevalence of Omicron or Delta during the study period. As described earlier, national data had shown that 87.5% of COVID-19 infections within London were due to the Omicron variant by 15th December 2021. Hence, the authors believe that the majority of infections in BAME patients were also Omicron. Other studies did not show any ethnic variation between Delta and Omicron infections either.18
This study demonstrates important differences in terms of mortality due to the Omicron variant as compared to previous studies examining COVID-19 mortality. Compared with previous studies from the same hospitals trust, this study showed that mortality rate post-COVID-19 was significantly lower than the previous two surges within this trust.19,20 Compared with 29.5% and 18.5% during the first two surges, respectively, only 13.7% of patients with COVID-19 died.20 For those with true COVID-19 (Group 1), the rate of 15.8% was still lower than previous reports. This study found only 26 deaths that were directly attributable to COVID-19 pneumonitis. This represents only 4.7% of all patients admitted with COVID-19. These are important observations as most mortality data from COVID-19 would include patients in all the three groups combined (13.7%) rather than those who truly died from COVID-19. The authors’ findings are consistent with other recent studies, which also found that Omicron infections caused less severe illness, with similar reductions in hospitalisations and death associated with Omicron infection.18,21,22 Moreover, this study showed that many deaths that may be classified as COVID-19-related were actually not directly attributable to COVID-19 pneumonitis.
Speculative reasons for improved outcomes in this study include the fact that the Omicron variant may be less virulent and aggressive in its effects compared to previous variants, including less endothilialitis;21 higher vaccination rates, which would reduce the impact of COVID-19 infections on the body; availability of better medical treatments, including steroids, antiviral therapy, and neutralising monoclonal antibodies; and more structured and faster processes for infection prevention and isolation, which meant fewer vulnerable patients may have been exposed to the risk. These results are in accordance with recent results published by the Office for National Statistics (ONS), which showed that the risk of death due to Omicron variant was 67% lower compared to the Delta variant in December 2021.23
This study showed that 52.0% of those admitted with COVID-19 pneumonitis were unvaccinated, and a further 22.5% had only had one or two vaccinations. While it may appear that only 52.0% of those admitted with COVID-19 pneumonitis were unvaccinated, implying that 48.0% had had at least one vaccination, it is important to compare these figures with the vaccination rates within the region at that time. As of 13th December 2021, there were 10.0–16.0% patients over 60 years who were unvaccinated (16.0% being 60–64 years and 10.0% being >80 years).24 These figures are important as the majority of the patients admitted were older than 60 years. Thus, this small proportion of patients in the local population contributed to over half of all admissions directly related to COVID-19. The vaccination status in Group 3 (75.0% had had between two and three vaccinations) is reflective of this cohort being predominantly an older, frailer cohort with multiple comorbidities, thus likely to have higher vaccination rates.
Limitations
There are some limitations to this study. The authors did not have information on the precise genotype of SARS-CoV-2 in these patients. Instead, they assumed it to be Omicron on the basis of prevalence data available for the population in the catchment area of the hospitals, which is in accordance with recent studies.7,8 The authors did not have any information on existing comorbidities of patients, which would have been useful in evaluating outcomes further. Whilst there were only three types of vaccines administered in the area served by the hospital prior to the period of the study (Pfizer–BioNTech COVID-19 vaccine, Oxford–AstraZeneca COVID-19 vaccine, and a very small proportion were administered the Moderna COVID-19 vaccine), there was no data available regarding the precise type of vaccine taken by the individual patients in this study. Therefore, the authors were unable to assess whether there were any differences in patient outcomes due to the type of vaccine administered. Finally, the authors do not have outcome data for the study for approximately 4.9% of patients who were still in hospital; however, it is unlikely that this missing data would have made any significant difference to the mortality rates identified in the study.
CONCLUSION
This large, multi-ethnic, hospital-based study has described the clinical presentations and mortality outcomes of hospitalised patients with the COVID-19 Omicron variant. It has determined socio-demographic factors associated with these presentations, including ethnicity and vaccination rates. The study provides information that may be useful in future COVID-19 studies examining outcomes and presentations of Omicron and future COVID-19 variants.








