Interviewees: Susanna Esposito,1 Jordi Vila,2 Gorm Lisby,3 Justin Chai4
1. Pediatric Clinic, Department of Medicine and Surgery, University of Parma, Italy
2. Department of Clinical Microbiology, Hospital Clinic of Barcelona, Spain
3. Department of Clinical Microbiology, University of Copenhagen, Hvidovre Hospital, Denmark
4. Emergency Department, Gleneagles Hospital Kota Kinabalu, Sabah, Malaysia
Disclosure: Esposito has received consultation honoraria from GlaxoSmithKline, QIAGEN, MSD, Pfizer, Sanofi, and Vifor. Vila has received research financial support from QIAGEN. Lisby has received project support and/or honoraria from bioMeriéux, QIAGEN, and STATdx. Chai has received consultation honoraria from QIAGEN.
Acknowledgements: Writing assistance was provided by Stevan Rakovic, Witney, Oxfordshire, UK.
Disclaimer: The opinions expressed in this article belong solely to the named interviewees. The QIAstat-Dx Meningitis/Encephalitis Panel (QIAGEN, Hilden, Germany) is indicated as an aid in the diagnosis of specific agents that cause meningitis and/or encephalitis, and results must be used in conjunction with other clinical, epidemiological, and laboratory data. Results from the QIAstat-Dx Meningitis/Encephalitis Panel are not intended to be used as the sole basis for diagnosis, treatment, or other patient management decisions. Positive results do not rule out co-infection with organisms not included in the QIAstat-Dx Meningitis/Encephalitis Panel. The agent or agents detected may not be the definite cause of the disease. Negative results do not preclude central nervous system infection. The QIAstat-Dx Meningitis/Encephalitis Panel is intended for in vitro diagnostic use by laboratory professionals only.
Support: The publication of this feature interview was supported by QIAGEN, who reviewed the article.
Citation: EMJ Microbiol Infect Dis. 2022;3[Suppl 1]:2-12. DOI/10.33590/emjmicrobiolinfectdis/10152446. https://doi.org/10.33590/emjmicrobiolinfectdis/10152446.
Keywords: Cancer, checkpoint inhibitor, chemotherapy, epigenetic, immunogenic, immunotherapy, medicine, oncolytic, radiotherapy, tumour, vaccine.
Meeting summary
Meningitis and encephalitis are serious diseases associated with considerable morbidity and mortality. Despite advances in vaccines and other preventative measures, meningitis remains a global public health challenge. Prompt and accurate diagnosis of meningitis and encephalitis are essential to allow early implementation of targeted therapy to minimise the risks of long-term disability and death. Conventional methods for the diagnosis of meningitis and encephalitis include brain imaging combined with evaluation of cerebrospinal fluid (CSF) by microscopy (using different staining procedures), cytochemical analysis, culture, and antigen detection; however, these diagnostic approaches have limitations. Molecular diagnostic techniques, such as multiplex real-time PCR (RT-PCR) panels, have been developed as point-of-care tests that facilitate the management of central nervous system infections.
In August 2022, EMJ conducted interviews with four key opinion leaders (KOL): Susanna Esposito from the University of Parma, Italy; Jordi Vila from the Hospital Clinic of Barcelona, Spain; Gorm Lisby from Hvidovre Hospital, Denmark; and Justin Chai from Gleneagles Hospital Kota Kinabalu, Malaysia, all of whom have a wealth of experience in the diagnosis and management of patients with meningitis or encephalitis. The experts provided important insights into the clinical investigations used to diagnose meningitis and encephalitis and their relative advantages and disadvantages. In addition, the experts described their experiences of using the QIAGEN QIAstat-Dx Meningitis/Encephalitis Panel (QIAGEN, Hilden, Germany), and they highlighted the potential advantages of multiplex RT-PCR panel testing compared with conventional diagnostic approaches.
INTRODUCTION
Inflammation of the meninges of the spinal cord and brain, or meningitis, and inflammation of the brain, or encephalitis, are usually caused by infection, and are associated with considerable morbidity and mortality.1 The most common causes of meningitis are viral infections followed by bacterial infections, while fungal and parasitic causes are rare.2 Encephalitis is most often due to viral infections, with bacterial and parasitic infections accounting for only a small number of cases.3 In 2016, there were more than 2.8 million cases of bacterial meningitis worldwide, and the incidence was highest in sub-Saharan Africa.4 Bacterial meningitis is a severe disease with a mortality rate of 10–15%.5,6 Furthermore, around 30% of children with bacterial meningitis experience neurological complications, including strokes; seizures; the development of focal neurological deficits such as hearing or vision loss; motor or sensory deficits; and speech, language, and communication impairment.7,8 The survival of patients with bacterial meningitis is improved by the prompt initiation of antibiotic therapy, and an increase in mortality is observed after a treatment delay of only 2 hours.9 Therefore, it is critical that meningitis and encephalitis are diagnosed rapidly and accurately so that appropriate therapy can be implemented as early as possible to minimise adverse clinical outcomes.
Conventional methods for the diagnosis of meningitis and encephalitis include analyses of CSF samples obtained by lumbar puncture and, in selected cases, brain imaging. CSF is examined for the presence of acute and chronic inflammatory cells by biochemical analysis of glucose and protein levels, Gram staining and microscopy for preliminary identification of bacterial organisms, and latex agglutination tests for bacterial antigens.2,10 In addition, CSF culture and antimicrobial susceptibility testing are used to identify bacterial pathogens, and singleplex RT-PCR assays are utilised to detect specific viruses.2,10 However, the conventional diagnostic tests for bacterial antigens have a slow turnaround time and limited sensitivity.11-13
Multiplex RT-PCR panel testing represents a relatively new approach to molecular diagnostics.14 The QIAstat-Dx Meningitis/Encephalitis Panel is a single test that can simultaneously detect 15 pathogens in around 1 hour.15 The micro-organisms identified by the QIAstat-Dx Meningitis/Encephalitis Panel include six viral, eight bacterial, and one fungal target, which together make up the most common pathogens associated with community-acquired meningitis and encephalitis.
For this article, four KOLs with expertise in diagnosing and managing meningitis and encephalitis, Esposito, Vila, Lisby, and Chai, discussed the conventional diagnostic methods and their limitations. They then described their experiences of using multiplex RT-PCR panel tests, including the QIAstat-Dx Meningitis/Encephalitis Panel. All four KOLs highlighted the advantages of multiplex RT-PCR panel testing, and explained how its use can facilitate the rapid and accurate diagnosis of meningitis and encephalitis to facilitate prompt implementation of the most appropriate and effective therapy, and thereby improve patient outcomes.
MAJOR CHALLENGES TO DIAGNOSING, TREATING, AND PREVENTING MENINGITIS AND ENCEPHALITIS
In 2021, the World Health Organization (WHO) published a global roadmap to defeat meningitis by 2030.16 The main aims of the WHO roadmap include eliminating epidemics of bacterial meningitis; reducing the number of vaccine-preventable bacterial meningitis cases by 50%; reducing the mortality from bacterial meningitis by 70%; and reducing disability and improving quality of life after meningitis due to any cause. The WHO roadmap acknowledges the challenges of diagnosing, treating, and preventing meningitis, and proposes 19 strategic goals spread across five pillars, which are prevention and epidemic control; diagnosis and treatment; disease surveillance; care and support of those affected by meningitis; and advocacy and engagement (Figure 1). Notably, WHO strategic goal 7 (pillar 2) recognises the importance of developing quality-assured, affordable, and accessible diagnostic assays, including multiplex RT-PCR panel tests, that can rapidly detect the main pathogens responsible for meningitis, since this will improve decision-making at the point of care. Furthermore, strategic goal 10 (pillar 3) proposes that up-to-date diagnostic tests should be used for the surveillance of the main causative pathogens. Therefore, implementing multiplex RT-PCR panel tests is expected to contribute to achieving the aims in the WHO roadmap.
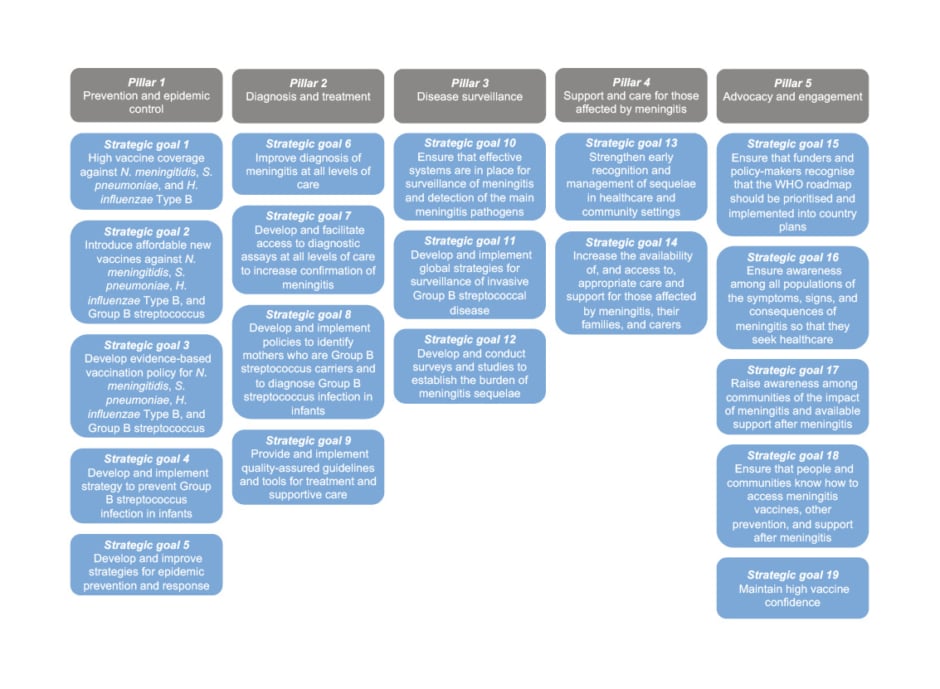
Figure 1: Summary of the World Health Organization (WHO) global roadmap to defeat meningitis by 2030.16
H. influenzae: Haemophilus influenzae; N. meningitidis: Neisseria meningitidis; S. pneumoniae: Streptococcus pneumoniae.
Esposito made several important points regarding the burden of meningitis and encephalitis. First, meningitis is an important global health problem with a mortality rate of around 10–15% and a disability rate of 20–30%, and outcomes are optimised if therapy for bacterial meningitis commences within 1 hour of symptom onset. Second, the war against meningitis can only be won through the prevention of infection, particularly with the implementation of vaccine programmes that cover the main causative pathogens. However, there are differences between European countries in the implementation of the pneumococcal vaccine in adults and the elderly (including those with chronic underlying diseases for whom pneumococcal vaccination is recommended) as well as the meningococcal B and meningococcal ACWY vaccines. Third, reducing the burden of meningitis and encephalitis will also require other goals to be met, including prompt diagnosis, timely intervention with appropriate therapy, and the implementation of measures to prevent the spread of infection in the community.
In addition, Esposito briefly mentioned the possible influence of the COVID-19 pandemic on meningitis and encephalitis. Specifically, although the number of cases of meningitis and encephalitis in developed countries fell during periods of lockdown because of reduced social contact, there was a decrease in vaccine uptake, particularly in adolescents and adults, and this may have increased the circulation of pathogens targeted by the vaccines. Esposito also raised the possibility that climate change might increase the circulation of some viruses, particularly those that show seasonal variation, and gave the example of the unusually large number of cases of West Nile virus meningitis in Italy during late August 2022.
Vila explained that the incidence of meningitis and encephalitis in Catalonia, Spain, was approximately five cases per million inhabitants in 2020. This low incidence was considered to be due to the implementation of the meningococcal C vaccine in 2000, pneumococcal vaccine in 2016, and meningococcal ACWY vaccine in 2020, as well as screening for meningitis-causing pathogens. For example, females who are pregnant are screened for Streptococcus agalactiae and, if needed, given antibiotic therapy during labour to prevent maternal transmission to the neonate. In 2017, enterovirus replaced Streptococcus pneumoniae as the most prevalent cause of meningitis in Catalonia, possibly following the vaccination programmes. According to Vila, three main challenges must be met to improve the diagnosis, treatment, and prevention of meningitis and encephalitis: introducing vaccination for group B meningococci into the schedule for children; making rapid diagnostic tests available in most diagnostic laboratories in Catalonia; and performing surveillance of antibiotic resistance among the main pathogens that cause meningitis and encephalitis.
Lisby discussed that the incidence of meningitis in Denmark showed some seasonal variation, but had remained largely unchanged during recent years. The main bacterial pathogens causing meningitis in Denmark were similar to those in other parts of northern and central Europe, including meningococci, pneumococci, and, in children, Escherichia coli, while the incidence of Haemophilus influenzae Type B meningitis had declined in Denmark due to a successful vaccination programme that was implemented in 1993. In Lisby’s view, the main challenge to preventing meningitis and encephalitis in Denmark is adherence to the vaccination programme, since several interest groups were against vaccination, while the main challenge to diagnosing and treating meningitis and encephalitis is access to rapid and sensitive diagnostics such as multiplex RT-PCR panel tests.
Chai explained that cases of meningitis and encephalitis are uncommon in Sabah, the second biggest state in Malaysia. They referred to a publication by Lee et al.,17 which reported 84 patients aged ≥12 years-old with suspected meningitis or encephalitis in Sabah between February 2012 and March 2013. Although the most common diagnoses reported by Lee et al.17 were tuberculous meningitis (48.8%) and cryptococcal meningoencephalitis (16.6%), the most recent cases of meningitis and encephalitis in Malaysia had been due to Japanese encephalitis virus, which is transmitted to humans by mosquitoes. Chai stated that efforts are being made to prevent the spread of Japanese encephalitis virus, including with home visits by public health professionals, to enhance awareness about disease transmission. They also highlighted the transportation problems faced by people who live in mountainous regions of Malaysia, which are inaccessible by vehicles. The ability to perform a rapid and accurate diagnosis at a local clinic would help to identify those patients who require transportation to a major hospital with the necessary facilities for high-dependency care and infection control.
THE IMPORTANCE OF RAPID AND ACCURATE DIAGNOSIS OF MENINGITIS AND ENCEPHALITIS
Patient Outcomes
All the experts agreed that a rapid and accurate diagnosis was essential to allow the implementation of specific therapy targeted at the causative pathogen. Vila elaborated that it is important to differentiate between bacterial, viral, and fungal causes of meningitis and encephalitis, because this allows for early intervention with appropriate therapy; for example, antibiotics for bacterial meningitis or aciclovir for herpes simplex virus (HSV) encephalitis. They stressed that mortality is higher for bacterial meningitis than for viral meningitis, and early treatment with antibiotics would reduce mortality and the incidence of neurological complications in patients with bacterial meningitis. Esposito agreed that a rapid diagnosis is particularly important in cases of bacterial meningitis because treatment within 1 hour of symptom onset can minimise the risks of complications and death. They explained that a delay in antibiotic administration is associated with increased mortality in patients with bacterial meningitis, and that treating HSV encephalitis with an antiviral agent can reduce the risk of mortality and other sequelae from 30% to 10%. Chai concurred that accurate diagnosis and provision of appropriate care must occur as soon as possible because central nervous system infections can progress rapidly, and potentially result in prolonged seizures, coma, cessation of breathing, and cardiopulmonary arrest. Lisby explained that all institutions have empirical treatment regimens that cover common bacterial causes of meningoencephalitis as well as HSV and varicella zoster virus (the two currently treatable viral causes of meningoencephalitis). According to Lisby, identification of the causative pathogen allows de-escalation of empirical antibiotics with more targeted treatment, especially in areas with low levels of antimicrobial resistance, or escalation to an appropriate antimicrobial treatment in rare cases where the pathogen is not covered by the empirical therapy (e.g., methicillin-resistant Staphylococcus aureus).
Adverse Events
Esposito explained that treatment with broad-spectrum antibiotics can be associated with adverse effects such as vomiting, diarrhoea, skin rashes, and a change in the gut microbiota. In addition, the management of meningitis complications, for example, with intubation or surgery, can also result in adverse events. Therefore, a prompt diagnosis and an early switch from empirical therapy to targeted treatment would be expected to reduce unnecessary antibiotic use and improve patient outcomes, thereby decreasing the incidence of adverse events. Chai agreed, stating that reducing the use of empirical antibiotics or antivirals would lower the incidence of adverse effects such as hepatotoxicity and renal toxicity.
Treatment Costs
According to Chai, a delay in diagnosing meningitis or encephalitis would also place burdens on hospital staff and healthcare systems. Vila suggested that an additional advantage of rapid diagnosis and targeted treatment might be lower treatment costs due to reduced length of hospital stay. Esposito added that a delay in treatment might also increase the incidence of long-term complications such as hearing loss and cognitive impairment, which can have a huge impact on the patient, and are associated with additional costs to healthcare systems.
Antimicrobial Resistance
Esposito suggested that diagnostic delay and use of an inappropriate treatment regimen can elevate the risk of an infection spreading in the community and increase the risk of drug resistance. Chai agreed that the empirical use of broad-spectrum antibiotics might promote the emergence of multidrug-resistant strains. However, Lisby disagreed, arguing that empirical therapy for meningitis and encephalitis has little impact on general antimicrobial resistance because the number of patients involved is too small to be a driver of antimicrobial resistance. They explained that antimicrobial stewardship aims to reduce the use of antimicrobials in patient populations that are not severely sick, thereby saving broad-spectrum antibiotics for severely ill patients for whom survival and long-term outcomes are directly correlated to the antimicrobial coverage and the speed at which treatment is initiated.
The experts agreed that drug-resistant strains could impact the treatment of meningitis and encephalitis because empirical therapy is ineffective if the pathogen is not susceptible to the antibiotics. Although Vila and Lisby described the prevalence of resistant strains as low in Spain and Denmark, other regions of the world have seen significant increases in antimicrobial resistance. Esposito and Vila stated that some parts of the world have experienced an increase in the number of cases of pneumococcal meningitis resistant to cephalosporins such as ceftriaxone or cefotaxime, which are first-line treatments for pneumococcal meningitis; therefore, empirical antibiotic therapy generally includes vancomycin or linezolid to cover any resistant organisms. Esposito added that Mycoplasma pneumoniae meningitis is quite common in children, and that quinolone antibiotics are required in these cases because macrolides do not penetrate well into the CSF, and because β-lactam antibiotics have limited efficacy against this bacterium. According to Vila, recent years have also seen a notable increase in the resistance of E. coli and Klebsiella to third-generation cephalosporins, particularly in regions such as Southeast Asia and India. All four experts concurred that rapid and accurate diagnosis allows for the early implementation of an appropriately tailored therapy, reducing the use of unnecessary antibiotics.
CONVENTIONAL METHODS USED TO DIAGNOSE MENINGITIS AND ENCEPHALITIS
The experts explained that the traditional diagnostic tools used by most laboratories include several tests on CSF samples obtained by lumbar puncture (Figure 2):2 cytochemical parameters, including leucocyte counts, glucose levels, and protein concentration, which help to differentiate between bacterial, viral, and fungal meningitis; Gram staining, which provides preliminary identification of a bacterial organism; Ziehl–Neelsen staining to identify acid-fast bacteria, including Mycobacterium; culture and antibiotic susceptibility testing; antigen testing to detect certain bacteria such as streptococci, meningococci, S. agalactiae, H. influenzae, and E. coli; and singleplex RT-PCR for enterovirus and HSV, as well as additional viruses when indicated (e.g., West Nile virus). According to the experts, blood cultures can support the diagnosis of meningitis; however, more than 12 hours are required for blood culture results to become available, and viruses cannot be detected using current methods. Neuroimaging was also mentioned as a complementary technique that visualises changes in the brain and meninges and identifies complications, but cannot be used to establish the underlying pathogen. Furthermore, Lisby pointed out that although neuroimaging may identify significant focal pathology, such as a cerebral abscess, it cannot confirm or exclude a diagnosis of meningitis or encephalitis.
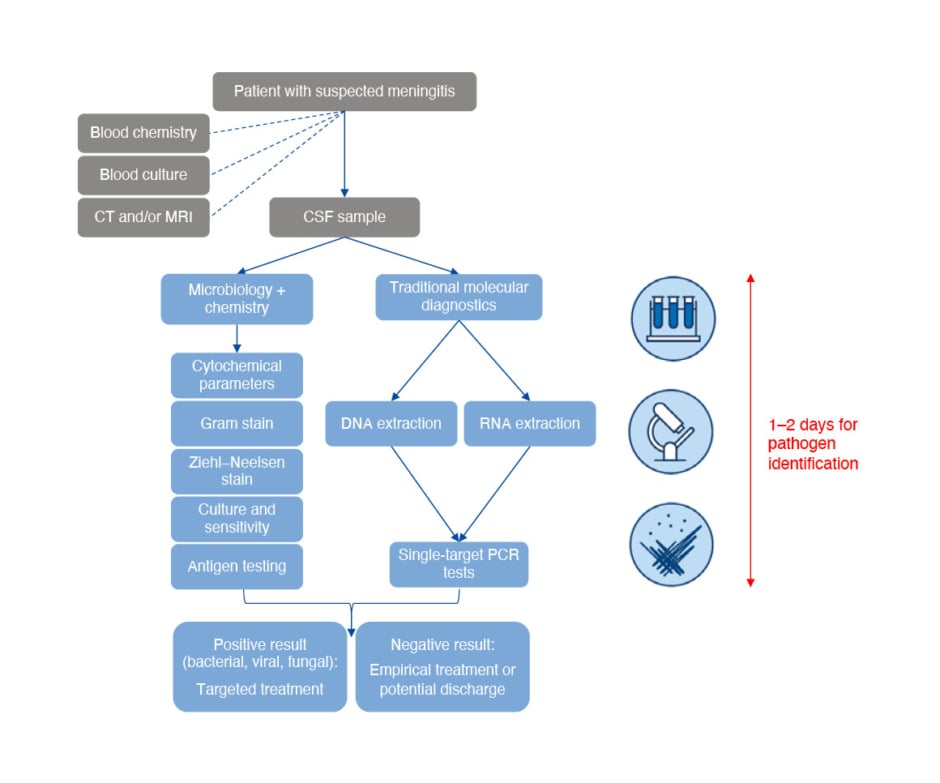
Figure 2: Conventional methods used to diagnose meningitis and encephalitis.
CSF: cerebrospinal fluid.
All experts agreed that slow turnaround was the most relevant disadvantage of CSF culture. Esposito explained that the results of CSF microscopy and cytochemical analysis are available in around 1 hour, whereas the CSF culture findings are usually obtained after 2 days. Chai revealed that it can take up to 2 weeks to obtain the results in public hospitals in Malaysia, which may have negative impacts on treatment outcomes if the empirical therapy does not cover the causative pathogen. This delay in diagnosis may also result in a higher risk of adverse events, longer length of hospital stay, and higher treatment costs, due to unnecessary use of antibiotics or antivirals during empirical therapy.
Another limitation of CSF culture described by Vila, Esposito, and Lisby is that the administration of antibiotics before lumbar puncture can result in a false negative result. According to Esposito, most cases of meningococcal meningitis are not diagnosed by CSF culture if a single dose of intravenous antibiotic is administered 1 hour before lumbar puncture.
Lisby explained that conventional diagnostic techniques are also limited by their low sensitivity and negative predictive value. Vila elaborated that the diagnostic sensitivity of Gram staining ranges from 25% to 30%, whereas microbial culture has a higher diagnostic sensitivity unless the patient has received prior antibiotic therapy. They stated that the sensitivity of antigen detection reaches 85–90%, but is lower than that of RT-PCR-based techniques and lower for certain organisms such as group B meningococci, which are not very antigenic. Another limitation of antigen detection mentioned by Vila is that it is only available for certain specific bacteria, and cannot identify all the main organisms that cause meningitis or encephalitis.
An additional issue raised by the experts is that conventional diagnostic techniques require several CSF-based tests to be run in parallel. Chai, Esposito, and Vila noted that a sufficiently large sample of CSF must be collected for the various conventional diagnostic tests, but this can be challenging in a patient with a small body size, especially when the patient is a neonate. Moreover, Chai and Lisby suggested that staffing costs would be higher for multiple conventional tests than for a multiplex RT-PCR panel test. However, Lisby noted that the total number of samples processed by each laboratory would be small enough to not have a major impact on the laboratory budget.
MULTIPLEX REAL-TIME PCR PANEL TESTS
QIAstat-Dx Meningitis/Encephalitis Panel
The QIAstat-Dx Meningitis/Encephalitis Panel is a multiplex RT-PCR test that can be used as an aid in diagnosing specific agents of meningitis and/or encephalitis. The QIAstat-Dx Meningitis/Encephalitis Panel can simultaneously detect 15 of the most common pathogens associated with community-acquired meningitis and encephalitis in around 1 hour. This panel includes E. coli K1, H. influenzae, Listeria monocytogenes, Neisseria meningitidis (encapsulated), S. agalactiae, S. pneumoniae, M. pneumoniae, Streptococcus pyogenes, enterovirus, HSV1, HSV2, human herpesvirus 6, human Parechovirus, varicella zoster virus, and Cryptococcus neoformans/gattii. The test requires a 200 µL sample of CSF, no sample manipulation, and a ‘hands-on’ time of only 1 minute. Additionally, the QIAstat-Dx system can provide a cycle threshold (Ct) value and an amplification curve for each detected pathogen.
The Role of Multiplex Real-Time PCR Panel Tests in the Diagnosis of Meningitis and Encephalitis
Vila explained that their hospital has been using the QIAstat-Dx Meningitis/Encephalitis Panel to aid the diagnosis of meningitis and encephalitis, and they emphasised that their hospital’s clinicians have been very happy with the rapidity of the system, which has allowed them to provide targeted therapy selected according to the results of the test, and thereby improve the management of their patients. Vila highlighted several important advantages of multiplex molecular diagnostics. First, a multiplex RT-PCR panel is a single test that can rapidly diagnose the most important bacterial, viral, and fungal causes of meningitis and encephalitis, in contrast to the conventional approach that relies on several different methodologies, each requiring a sample of CSF. Second, the availability of a rapid result allows targeted therapy to be implemented early, thereby reducing the unnecessary use of antibiotics. Third, molecular diagnostic techniques can identify bacterial organisms in patients who received antibiotic therapy before lumbar puncture. In addition, Vila speculated that using rapid molecular diagnostics would allow better control of potential outbreaks (e.g., of N. meningitidis) in the hospital and community, because infection control measures could be implemented early. Despite multiplex RT-PCR panel tests not including all the possible pathogens that cause meningitis or encephalitis (e.g., Pseudomonas aeruginosa or S. aureus), Vila proposed that rapid multiplex RT-PCR panel tests should be implemented into the workflow of most laboratories.
Esposito also described several notable advantages of multiplex RT-PCR panel tests, including speed, the detection of bacterial pathogens in patients previously treated with antibiotics, and the requirement of only a small volume of CSF. Since meningitis is an emergency, Esposito suggested that multiplex RT-PCR panel tests should be used for all cases where meningitis or encephalitis is suspected, and a lumbar puncture is performed. Esposito considered it essential that the emergency room and wards have access to a multiplex RT-PCR panel test so that a rapid result can be obtained in patients with suspected meningitis or encephalitis.
Lisby explained that the QIAstat-Dx Meningitis/Encephalitis Panel was being evaluated against their current diagnostic panel, the BioFire® FilmArray® Meningitis/Encephalitis Panel (BioFire Diagnostics, Salt Lake City, Utah, USA). Although the emergence of molecular-based diagnostics had greatly improved the diagnosis of meningitis and encephalitis, Lisby emphasised that a negative result from a RT-PCR-based test could not be used alone to rule out these diseases, or justify treatment discontinuation. Nevertheless, the multiplex RT-PCR panel test was used in their institution whenever there was clinical suspicion of meningitis or encephalitis, and the infectious disease specialist requested the test. Lisby suggested that one advantage of multiplex RT-PCR panel tests over conventional diagnostic techniques is a lower risk of sample contamination during handling in the laboratory. In their view, the diagnosis of meningitis and encephalitis is one of the few instances where implementation of a multiplex RT-PCR panel test is merited without health economic outcome studies, which are required in other syndromic diseases such as pneumonia or sepsis. The reason for this is that because the overall number of patients with suspected meningitis and encephalitis is small, and the clinical outcome potentially so dramatic, there is already a sound business case for implementing rapid diagnostic testing to facilitate the early initiation of targeted therapy. Nevertheless, Lisby did not envisage multiplex RT-PCR panels replacing conventional culture in the foreseeable future due to the need for phenotypic antimicrobial susceptibility testing.
Chai stated that their hospital’s laboratory runs multiplex RT-PCR panel tests, and that they have used the QIAstat-Dx Meningitis/Encephalitis Panel on a couple of occasions. Several advantages of multiplex RT-PCR panel tests over conventional methods were highlighted, including rapidity, ease of use, and coverage of the main pathogens associated with meningitis and encephalitis. Chai described the benefits of multiplex RT-PCR panel tests from the perspective of three major stakeholders, including the patient, the treating clinician, and the hospital or healthcare system. The advantages for patients include better prediction of prognosis once the underlying pathogen is identified, and improved outcomes due to earlier intervention with targeted therapy. One benefit to clinicians is that rapid and accurate identification of the pathogen would allow the physician more time to focus on supportive management, such as improving ventilation, preventing ventilator-acquired pneumonia, and preventing ulcer development in bedridden patients. Using rapid diagnostics might also enable clinicians to improve antibiotic stewardship and reduce the risk of multidrug-resistant pathogens emerging. Multiplex RT-PCR panel tests may benefit healthcare systems by establishing strong trust between the patient and hospital, since the patient would be aware that the hospital was running the most efficient diagnostic tests and providing the best supportive care it could. Establishing this trust is important because it encourages patients to seek medical help when they feel unwell. Chai went on to describe an interesting case of a patient in which the QIAstat-Dx Meningitis/Encephalitis Panel correctly diagnosed varicella zoster meningitis despite the absence of a characteristic vesicular rash, which appeared the following day.
Cycle Threshold Values and Amplification Curves
The Ct value of an RT-PCR reaction describes the cycle number at which the measured fluorescence signal exceeds a calculated background threshold. A lower Ct value has been reported to be a significant predictor of the emergence/progression of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreaks, the risk of developing severe COVID-19 illness, and SARS-Cov-2 infectiousness.18 Furthermore, there is evidence that a low Ct value may be associated with more severe symptoms and poorer outcomes in patients with gastrointestinal infections.19 Hence, it has been suggested that a lower Ct value may be indicative of a higher pathogen load. In addition, the amplification curve can help to confirm the success of the RT-PCR reaction, thereby providing confidence in the results.
Lisby strongly believed that Ct values and amplification curves from multiplex RT-PCR panel tests could help to support the diagnosis and management of patients with suspected meningitis or encephalitis. They explained that although contamination is not a major issue in meningitis diagnostics, positive molecular test results are occasionally returned that are not consistent with the clinical presentation (e.g., a human herpesvirus 6-positive signal in the absence of matching clinical symptoms). However, without access to the Ct value or amplification curve, it is not possible to evaluate whether such a result is a strong positive (suggesting the presence of the infection in the patient) or the consequence of potential contamination or a suboptimal RT-PCR reaction. Lisby stated: “I cannot stress clearly enough and strongly enough that Ct values and amplification curves are a must whenever we implement any molecular test for any disease.” Although their laboratory had implemented some ‘black box’ tests that do not provide access to Ct values and amplification curves, the intention is to replace these tests as soon as possible with alternatives that do provide this information, because this will allow results to be interpreted at a more professional level, and clinicians to receive better guidance in comparison to a black box approach.
Vila confirmed that their laboratory checks the amplification curve when the Ct value is high (e.g., ≥35) because, in their experience, the amplification curve sometimes shows the result to be a false positive. Vila also referred to the ongoing debate regarding the utility of Ct values in diagnosing meningitis and encephalitis, as well as other infectious diseases such as those of the gastrointestinal and respiratory systems, including COVID-19. Specifically, it was suggested that the Ct value could potentially be used as an indirect indicator of microbial load in a CSF sample because CSF is a liquid that is far less heterogeneous than, for example, a nasopharyngeal swab specimen or a stool sample. Lisby agreed that the Ct value might provide semi-quantitative information that correlated with clinical outcome, because there may be an association between pathogen load and clinical outcome in meningitis. However, Lisby emphasised that the Ct value does not provide an accurate estimation of the pathogen load, because this would require a quantitative system with standard curves. Therefore, further studies are needed to evaluate the associations between Ct value or pathogen load and the severity or prognosis of meningitis or encephalitis.
Esposito argued that, from the perspective of the treating clinician, a single Ct value is not particularly useful for evaluating cases of meningitis or encephalitis because the CSF is normally a sterile site; therefore, the presence of a pathogen is enough to indicate infection. Nevertheless, Chai speculated that the Ct value and amplification curve might be helpful in rare cases where meningitis is due to multiple organisms in the same patient, because this information might give some insight into the predominant causative organism.
FUTURE PROSPECTS AND CONCLUSIONS
Chai concluded that molecular diagnostics allow specific treatments to be rapidly administered to reduce the risks of complications, morbidity, and mortality. In their view, multiplex panel tests should replace conventional tests in due course because accurate results are obtained quickly, allowing the treating physician to select the optimal management strategy in a timely manner. They suggested that molecular panel tests represent the future of diagnosis, and are an important step towards implementing precision medicine for diseases such as meningitis and encephalitis. Although there is a long road ahead to achieving these goals, the functionality of rapid molecular diagnostic testing with a multiplex panel provides a step forward in the right direction.
Given their positive experiences with multiplex RT-PCR panel tests, Vila concluded that studies are required to establish the benefits of this molecular diagnostic technique in patients with meningitis or encephalitis. Specifically, research should be undertaken to determine whether CSF cytochemical parameters could be used to select patients for multiplex RT-PCR panel testing, and establish the clinical impact of multiplex molecular diagnostic techniques. Vila also proposed that a study should be carried out to analyse the cost-effectiveness of implementing multiplex RT-PCR panel testing in the workflow of the laboratory, taking into consideration factors such as the use of unnecessary antibiotics during empirical therapy, and the length of hospital stay.
Lisby concluded the interview by emphasising the importance of having access to Ct values and amplification curves. They explained that an ideal test would be capable of ruling out meningitis or encephalitis, but because such a test would require a sensitivity of 100%, it is unlikely that it will ever be developed. Therefore, in their view, the next significant development in diagnostics will be to look at the host immune response as an indicator of the presence and severity of infection.
Esposito concluded that multiplex RT-PCR panel tests should be available to clinicians in all major hospitals. They also proposed studies to analyse the cost-effectiveness of multiplex RT-PCR panel tests and their possible benefits to patients in terms of outcomes, as this information will be needed for the widespread implementation of this diagnostic technique. Since the COVID-19 pandemic and associated lockdowns may have resulted in changes in the circulating pathogens, Esposito also recommended multicentre studies to evaluate the epidemiology of meningitis and encephalitis in different age groups. Additionally, they advocated research to compare diagnostic performance and patient outcomes between multiplex RT-PCR panel tests and conventional CSF culture.








