INTRODUCTION
Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a rare systemic autoimmune disease with a yearly incidence rate of around 20 in 1million people. This is a challenging disorder causing substantial morbidity and is often life-threatening.1-6 In order to increase Hungarian nephrologists’ vigilance around the disease, and to provide comparative epidemiological and outcome data, the Hungarian Society of Nephrology established the Hungarian Vasculitis Registry in 2013. All Hungarian nephrology centres were asked to participate in data collection of patients with AAV.
AIMS AND METHODS
A custom-made web interface was developed for anonymised patient data collection. Clinical and laboratory results, as well as histological renal biopsy results and immunosuppression (ISU) data, were documented. Follow-up data concerning disease activity, remission, relapse, renal function, need for renal replacement therapy, induction and maintenance of ISU, and cause of death were also registered.
RESULTS
Since the interface’s initiation, these registry data of 334 patients have been collected. Their mean age was 58.5 years, 64% of which were female. 34% had cytoplasmic type ANCA, 59% perinuclear type ANCA, 2% positivity for both, and 5% proved to be ANCA negative. Renal biopsy showed focal, diffuse crescentic, mixed, and sclerotic histological classes in 28%, 36%, 29%, and 7% of patients, respectively. At baseline, the estimated glomerular filtration rate was 18.5 mL/min, and 31% of the patients required renal replacement therapy (RRT). Following ISU induction, 24% of the initially dialysed patients recovered renal function. Of those who did not need RRT at diagnosis, 15% developed end-stage renal disease during follow-up. Predictors of RRT were diffuse or mixed histology (OR: 10.5, p<0.001; and odds ratio (OR): 3.22, p=0.013, compared to focal, respectively) and the presence of skin lesions (OR: 3.1, p=0.012). Presence of joint involvement seemed to be protective (OR: 0.34, p=0.002). The induction and maintenance ISU are summarised in Figure 1. Remission was achieved in 83% of patients.
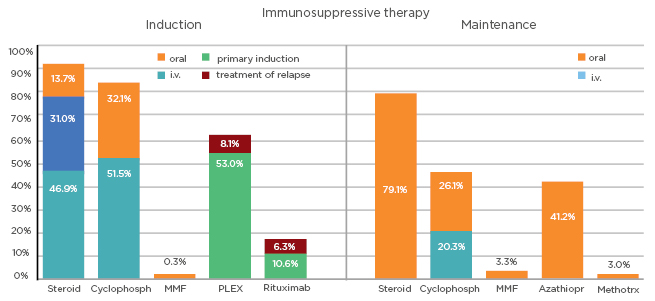
Figure 1: Immunosuppressive therapy for the induction and maintenance of antineutrophil cytoplasmic antibody-associated vasculitis.
Azathiopr: azathioprine; Cyclophosph: cyclophosphamide; i.v.: intravenous; Methotrx: methotrexate; MMF: mycophenolate mofetil; PLEX: plasma exchange.
During the median follow up of 30 months, 20% of patients died and 6% required transplant. The 1-year, 5-year, and 10-year survival rates were 94%, 82%, and 69%, respectively. Long-term survival appeared better in patients with cytoplasmic type ANCA compared to perinuclear type ANCA positive patients, but this difference disappeared by correcting for age. Predictors of death were age (hazard ratio [HR]: 1.86, p<0.001, for 10 years increment) and requirement of dialysis (HR: 2.98, p<0.001). Female sex (HR: 0.52, p=0.024) and steroid maintenance therapy (HR: 0.37, p=0.003) were protective factors. Relapse developed in 29% of patients, with risk decreasing by age (OR: 0.74, p=0.001), and plasma exchange as part of ISU induction (OR: 0.54, p=0.019). The risk of relapse was higher with lower respiratory symptoms (OR: 1.73, p=0.038).
DISCUSSION
As reflected by the increasing number of yearly reported patients, the Hungarian Vasculitis Registry helps growing nephrologists’ awareness of this rare disease and also provides opportunity for quality control. The documented epidemiological and clinical characteristics are comparable to other countries’ registry data, and underline the importance of early diagnosis to achieve the best outcome for patients.








