BACKGROUND AND AIMS
Eosinophilic granulomatosis with polyangiitis (EGPA) is a systemic necrotising vasculitis affecting small to medium sized vessels, characteristically associated with asthma and eosinophilia.1-3 Renal involvement occurs in approximately 25% of EGPA cases.4,5 Presentation includes focal and segmental necrotising crescentric glomerulonephritis (NCGN),4,6 eosinophilic interstitial infiltrates,4,7 or obstructive uropathy4 caused by vasculitic involvement of the ureters. The aim of this study was to analyse the prevalence, clinical manifestations, and outcomes of EGPA patients with renal involvement.8
METHODS AND RESULTS
The authors retrospectively analysed 142 patients with EGPA classified using American College of Rheumatology (ACR) and consistent with Chapel Hill Consensus 2012 definitions. Patients were selected with renal involvement defined by the presence of A) renal insufficiency serum creatinine (SCr) >97 uMol/L, or B) haematuria and/or proteinuria (>1+ in urinalysis), or C) obstructive uropathy.
Eleven (7.74%) patients with renal involvement (Table 1), 8 men and 3 women, with a mean age of 58.3±8.8 years, were identified. Median time of follow-up was 10.8±9.5 years. Seven were anti-neutrophil cytoplasmic antibody (ANCA) positive, six with myeloperoxidase (MPO), and one proteinase 3 (PR3)–ANCA. Three presented with rapidly progressive kidney injury with SCr >290 uMol/L, six with SCr >117 uMol/L, and two had normal SCr (44–97 uMol/L). Data for dipstick analysis on ten patients revealed seven with haemoproteinuria, one with proteinuria, and two with normal urinalysis. Renal biopsy was performed in six patients, showing three with NCGN, two had both NCGN and tubulointerstitial nephritis (TIN) with eosinophil infiltrates, and one had TIN with eosinophil infiltrates alone. All the patients with NCGN were ANCA positive, while the patient with TIN alone was ANCA negative. Two patients had obstructive uropathy due to ureteric stenoses. Patients received immunosuppressant therapy with prednisolone, cyclophosphamide, rituximab, mycophenolate mofetil, azathioprine, methotrexate, and plasma-exchange (Table 1). At the end of follow-up, two patients were renal transplant recipients, five had chronic kidney disease, and four maintained normal kidney function.
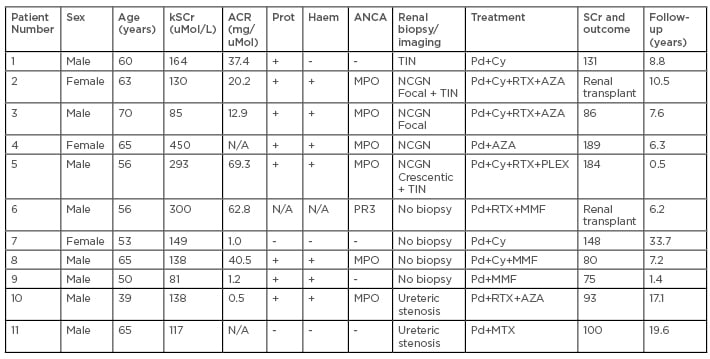
Table 1: Renal Involvement in eosinophilic granulomatosis with polyangiitis.
ACR: albumin creatinine ratio; ANCA: anti-neutrophil cytoplasmic antibody; AZA: azathioprine; Cy: cyclophosphamide; EGPA: eosinophilic granulomatosis with polyangiitis; Haem: haematuria in dipstick; MMF: mycophenolate mofetil; MPO: myeloperoxidase; MTX: methotrexate; N/A: not applicable; NCGN: necrotising crescenteric glomerulonephritis; Pd: prednisolone; PLEX: plasma exchange; PR3: proteinase 3; Prot: protein dipstick; RTX: rituximab; SCr: serum creatinine; TIN: tubulointerstitial nephritis.
CONCLUSION
While renal involvement in EGPA is less frequent than in other ANCA-associated vasculitic (AAV) subgroups, vigilance for its presence is required given its potential to lead to end-organ failure. The literature reports 10% of patients with renal AAV (microscopic polyangiitis/GPA/EGPA) disease are ANCA negative,1 the authors observed 36% ANCA negative EGPA patients with renal disease. Ureteric stenosis and eosinophilic TIN in this group raises awareness of the non-glomerular and extra-renal manifestations associated with EGPA.4,7 Necrotising crescentric nephritis was observed in isolation and also with concomitant TIN, opening the dialogue for the possible role of eosinophilic activation for the development of renal disease in EGPA.4 Furthermore, all patients in this group were ANCA positive, in keeping with previous studies.9 The predominant specificity, as expected for EGPA, was MPO–ANCA.
Further investigation to assess if ANCA negativity is associated with an eosinophilic infiltrative and granulomatous disorder involving the interstitium and urological tract, while ANCA positivity progresses to a necrotising glomerular disorder typical of all AAV, is of interest. Along with crescentic glomerular disease, tubular interstitial disease as a sole entity can lead to renal injury. Steroid therapy for other manifestations may mask renal disease. The authors draw attention to urological and renal manifestations of EGPA, and the presence of two patients requiring renal transplantation underscores the importance of renal Investigation in EGPA.10








