For many years, force platforms and centre of pressure biofeedback were used as tools for static balance training. However, thanks to motion tracking systems based on depth cameras, in recent years it has become possible to track not only the pressure centre but also the entire body and centre of mass. The most well-known of these sensors is the Microsoft Kinect™ (Redmond, Washington, USA), which, according to many studies, has sufficient accuracy of recording movements for clinical use.1 Additionally, for successful correction of any movement, there must be an external focus of attention.2 Virtual reality training can provide task-oriented motion training with full body biofeedback, based on three-dimensional (3D) motion capture data, with motivating gaming exercise.
In this study, patients with chronic cardiovascular disease and moderate balance disturbances were enrolled. Our goal was to investigate the effect of 3D balance training in virtual reality environments and compare the results to conventional training, which comprised individual sessions of vestibular exercise therapy with a physical therapist. To assess the efficacy, we used clinical scales and a built-in instrumental Romberg test, based on centre of mass displacement data.
For static balance training, a darts exercise was used in which the patient could control the aim of the dart by moving their centre of mass; 5 seconds after a dot appears the dart is fired at the target. The aim of another static exercise was to avoid flying balls by translating centre of mass in the frontal plane. Training of dynamic balance aimed to improve stability by prompting the patient to perform side and forward steps. For this, three exercises were chosen: dodging flying balls by performing side steps, stepping over the crossbar and placing the foot on the emerging track, and beating the rolling balls with one foot. The preliminary data showed significant improvements in Berg balance scale (p<0.05) (Figure 1) and single support phase during forward stepping, as well as decreased oscillations (p<0.05) during the Romberg test in the study group. In the control group, significant changes were observed only in static balance measured with Berg balance scale; the Romberg test showed only a trend of improvement.
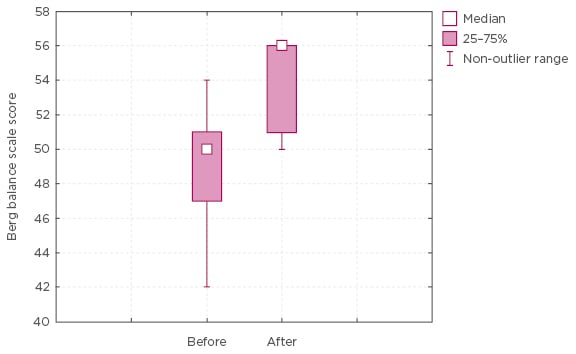
Figure 1: Berg balance scale scores in the main group before and after the treatment course.
We believe that the study group showed the best outcomes due to 3D feedback. The third-person view provided full body biofeedback and helped patients learn how to better control the position of their body in space. On the other hand, in early research it was shown that both the observation and imitation of intransitive actions seen from a first-person perspective yielded increased activity of the contralateral sensory-motor cortex compared to the same actions perceived from a third-person perspective.3 We can assume that the efficacy of the type of view in a virtual environment depends on the type of trained task. For example, for the training of hand and leg movements, the most effective perspective is the typical first-person view. On the other hand, for balance training, the physiological first-person view, which provides visual feedback about the position of the surroundings, may not be an informative stimulus for the patient; therefore, a third-person view can be more effective in balance training. This assumption needs further study and validation using a Kinect Romberg test. Further research is also of interest to compare the accuracy of registration and rehabilitation efficacy of separate use of the Kinect sensor and stabiloplatforms, as well as their combinations.








