BACKGROUND AND AIMS
Patients with classic orthostatic hypotension (cOH) suffer from an abnormally large blood pressure (BP) fall upon standing due to baroreflex dysfunction. cOH, particularly in the absence of BP-lowering drugs, often has a neurogenic cause (neurogenic orthostatic hypotension [nOH]). In approximately half of all patients with nOH, this coincides with supine hypertension (i.e., systolic BP [SBP] ≥140 mmHg, diastolic BP ≥90 mmHg, or both);1 however, the underlying mechanisms of this complication are poorly understood.2 Supine hypertension is thought to aggravate low BP complaints in cOH due to increased overnight pressure natriuresis, resulting in relative hypovolaemia in the morning.1,3 Supine hypertension is a risk factor for cardiovascular disease in the general population and it is also associated with increased cardiovascular risk in nOH.3,4
The authors aimed to investigate the haemodynamic mechanisms of supine hypertension in patients with cOH.
MATERIALS AND METHODS
The authors performed a retrospective analysis of continuous BP patterns in 65 patients with cOH (53 of these individuals had nOH) and 39 age-matched controls who underwent a tilt test. The authors compared the means of two periods: -180 seconds to -20 seconds before and 170 seconds to 190 seconds after the head-up tilt. Modelflow was used to analyse mean arterial pressure (MAP) and its constituent heart rate, stroke volume (SV), and total peripheral resistance (TPR). Both groups were split based on the median supine SBP of 150 mmHg, dividing them in a high supine SBP group and a low supine SBP group.
RESULTS
Patients with cOH and a relative high supine SBP, and therefore MAP, had a significantly higher supine TPR than those with a relative low supine SBP (p<0.0001), while supine heart rate and SV did not differ between groups (Figure 1). The upright position yielded a more pronounced MAP fall (p<0.0001) and smaller SV decrease (p=0.001) in those patients with cOH and higher supine BP relative to those with lower supine BP. Notably, in those with cOH and high supine SBP, the larger BP fall upon tilting was not accompanied by a more marked TPR response, suggesting a ceiling effect of TPR in this group (Figure 1). Interestingly, when comparing the relative high and relative low supine SBP control groups, the authors did not find contrasts in either supine or standing TPR.
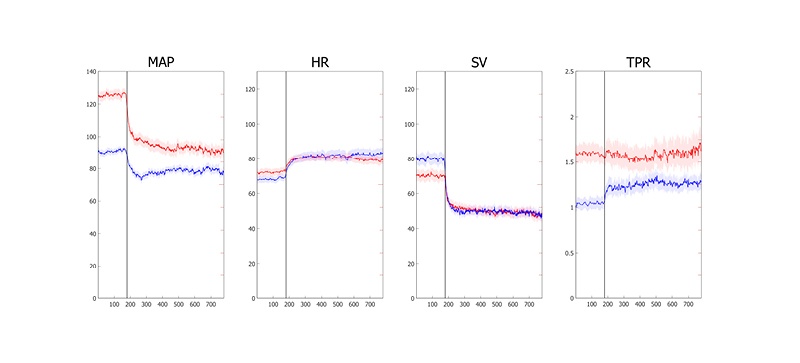
Figure 1: Time course of haemodynamic parameters in patients with classic orthostatic hypotension according to supine systolic blood pressure.
Lines indicate average±standard error, the point of tilt is indicated by the horizontal line visible at 180 seconds.
Red: high supine systolic blood pressure; blue: low supine systolic blood pressure.
HR: heart rate; MAP: mean arterial pressure; SV: stroke volume; TPR: total peripheral resistance.
CONCLUSION
Supine hypertension in cOH is primarily driven by a high TPR in supine position and a larger BP fall caused by an inability to increase TPR beyond supine levels, which is slightly counteracted by a smaller decrease in SV. Supine hypertension in nOH may result from long-term influences affecting BP homeostasis. The inability to increase TPR upon standing suggests more widespread baroreflex failure. Non-autonomic humoral mechanisms could be considered to explain the relative high supine TPR in supine hypertension and nOH.








