OBJECTIVE
To evaluate the outcomes of a three-week interdisciplinary intensive outpatient treatment program for mild-moderate traumatic brain injury (TBI) in veterans and first responders.1
BACKGROUND
Military service members and first responders are at elevated risk for TBI. While most individuals with mild TBI report no persisting symptoms >6 months post-injury, approximately 15% experience persisting cognitive, mood, and/or somatic consequences. Currently, there is no standard of care for treating persistent symptoms associated with mild-to-moderate TBI.
METHODS
The Haley Brain Wellness Program (HBWP) is a 3-week, interdisciplinary outpatient treatment program for veterans and first responders with persisting symptoms from TBI. Descriptive statistics and paired samples t-tests were conducted to examine intensive outpatient program (IOP)-associated changes in self-reported neurobehavioral symptoms, as well as measures of cognitive, vestibular, and sensory-integration functioning, for 128 participants (Table 1).
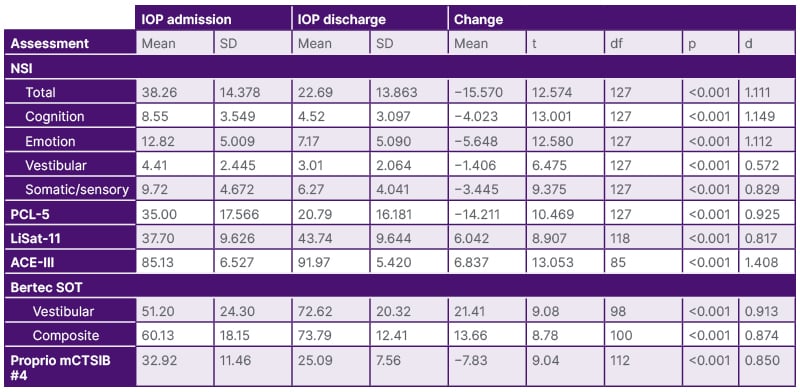
Table 1: Selected results from patient-reported and objective clinical outcomes at the start and end of the 3-week intensive outpatient program.
ACE-III: Addenbrooke’s Cognitive Examination-III; IOP: intensive outpatient program; LiSat-11: Life Satisfaction Questionnaire-11; mCTSIB: Modified Clinical Test for Sensory Interaction on Balance; NSI: Neurobehavioral Symptom Inventory; PCL-5: Posttraumatic Stress Disorder Checklist for DSM-5; SD: standard deviation; SOT: sensory organization test.
RESULTS
The majority of attendees were male (81%, n=104). The average age was 49 years (standard deviation [SD]:11.7, range: 23–78). The average time since the last TBI with loss of consciousness was 18.4 years (SD:13.9), with 76% of individuals reporting any TBI with loss of consciousness. Upon discharge, HBWP participants reported a mean decrease of 15.570 points (41%) on the Neurobehavioral Symptom Inventory (NSI; Cohen’s d=1.111). Scores on Addenbrooke’s Cognitive Examination-III (ACE-III) improved by an average of 6.837 points (Cohen’s d=1.408). Furthermore, participants increased their forward (Cohen’s d=0.679) and reverse gait speed (Cohen’s d=0.758), and demonstrated large improvements on tests of sensory integration (Bertec sensory organization test [SOT] composite; Cohen’s d=0.874) and vestibular function (Proprio-mCTSIB#4; Cohen’s d=0.850).
CONCLUSION
The HBWP model demonstrates strong preliminary efficacy in reducing symptoms associated with mild-moderate TBI and improving performance on clinical measures of cognition, vestibular function, and sensory integration. These results have implications for the development of a standard of care for persistent post-TBI symptoms in this patient population.
Further studies are necessary to determine whether these short-term results are sustained over time.







