Abstract
Introduction: Reversible cerebral vasoconstriction syndrome (RCVS) is a rare and underdiagnosed cause of multifocal infarcts, characterized by transient segmental
narrowing of cerebral arteries. This case highlights the diagnostic challenges, as well as the therapeutic response to nimodipine and intra-arterial therapy.
Main Symptoms and Clinical Findings: A 54-year-old female presented with a month-long history of confusion, headaches, and weakness. MRI findings revealed multifocal infarcts
across multiple vascular territories.
Main Diagnoses, Therapeutic Interventions, and Outcomes: RCVS was diagnosed following a diagnostic cerebral angiography, which demonstrated the reversibility of vasospasm with intra-arterial milrinone and verapamil. Treatment with nimodipine resulted in symptom stabilization, and rehabilitation services were initiated.
Conclusion: This case underscores the need to consider RCVS early in the diagnostic process for multifocal infarcts. Rapid identification through angiography and prompt initiation of nimodipine therapy can prevent unnecessary interventions and support meaningful neurological recovery.
Key Points
1. Reversible cerebral vasoconstriction syndrome can mimic more common pathologies like central nervous system vasculitis or infection, and is often underrecognized.
2. Accurate diagnosis of reversible cerebral vasoconstriction syndrome relies on imaging techniques such as cerebral angiography, which can demonstrate reversible vasospasm, a key diagnostic hallmark.
3. Prompt treatment with calcium channel blockers, such as nimodipine, is essential to both prevent further neurological damage and improve outcomes. Early diagnosis reduces the risk of overtreatment with immunosuppressants and improves functional outcomes.
INTRODUCTION
Reversible cerebral vasoconstriction syndrome (RCVS) is a rare, but critical diagnosis in patients presenting with recurrent, thunderclap headaches, and multifocal infarctions.1,2 Misdiagnosed as central nervous system vasculitis or infection, RCVS is typified by segmental cerebral arterial vasoconstriction that resolves spontaneously or with targeted therapeutic regimens.3 The diagnostic and therapeutic pathway of a 54-year-old female patient with RCVS, and the utmost significance of proper diagnosis and management of this condition, are both demonstrated in this article.
PATIENT INFORMATION
The patient is a 54-year-old woman living in Ontario. She is independent in daily activities, with occasional support from her daughter.
Primary Concerns and Symptoms
The patient was admitted to the hospital with a history of confusion, progressive headaches, and a weakness in the legs that had started 1 month prior. The symptoms evolved into expressive aphasia and right hemianopsia.
Medical, Family, and Psychosocial History
The patient had generalized anxiety disorder and bipolar disorder in her medical history. She also had a 20+ pack-per-year smoking history with a current daily use of cannabis and a recent smoking cessation.
Relevant Past Interventions
Past interventions included recent treatment with psychotropic medications for her mental health conditions, and two prior emergency department visits for similar symptoms, where initial investigations were inconclusive.
CLINICAL FINDINGS
The physical exam was notable for detecting expressive aphasia, right hemianopsia, and difficulty with word finding. The neuro exam was otherwise unremarkable. Vital signs were stable without any apparent cardiovascular or pulmonary disease.
TIMELINE
In September 2024, the patient initially presented with weakness and confusion, and a CT scan of the head was negative for any acute process (Figure 1). By late September 2024, MRI imaging demonstrated multifocal infarcts, leading to the initiation of antibiotic therapy for a presumed central nervous system infection. In October 2024, a diagnostic cerebral angiogram confirmed RCVS, and the patient was started on nimodipine.
Figure 1: Non-contrast head CT.
An axial, non-contrast CT of the brain performed at initial presentation demonstrates no evidence of acute hemorrhage, mass effect, or ischemia. The ventricular system and sulci are preserved, with no signs of raised intracranial pressure or midline shift. These findings contributed to a delay in diagnosis, emphasizing the limitation of an early CT scan in reversible cerebral vasoconstriction syndrome evaluation.
DIAGNOSTIC ASSESSMENT
The patient’s MRI imaging revealed multifocal infarcts with evolving features (Figure 2A/2B). A cerebral angiography thereafter confirmed the presence of segmental vasospasm and demonstrated reversibility following intra-arterial administration of milrinone and verapamil. Extensive infectious and autoimmune panels were negative.
The main diagnostic challenge was the resemblance of RCVS to vasculitis and central nervous system infections, which led to an initial misdiagnosis and delays in targeted therapy. Additionally, access to advanced neurointerventional studies was limited. The final diagnosis was RCVS with multifocal infarcts secondary to cerebral vasospasm. The patient’s prognosis was stable upon discharge with continued nimodipine therapy and multidisciplinary rehabilitation support.
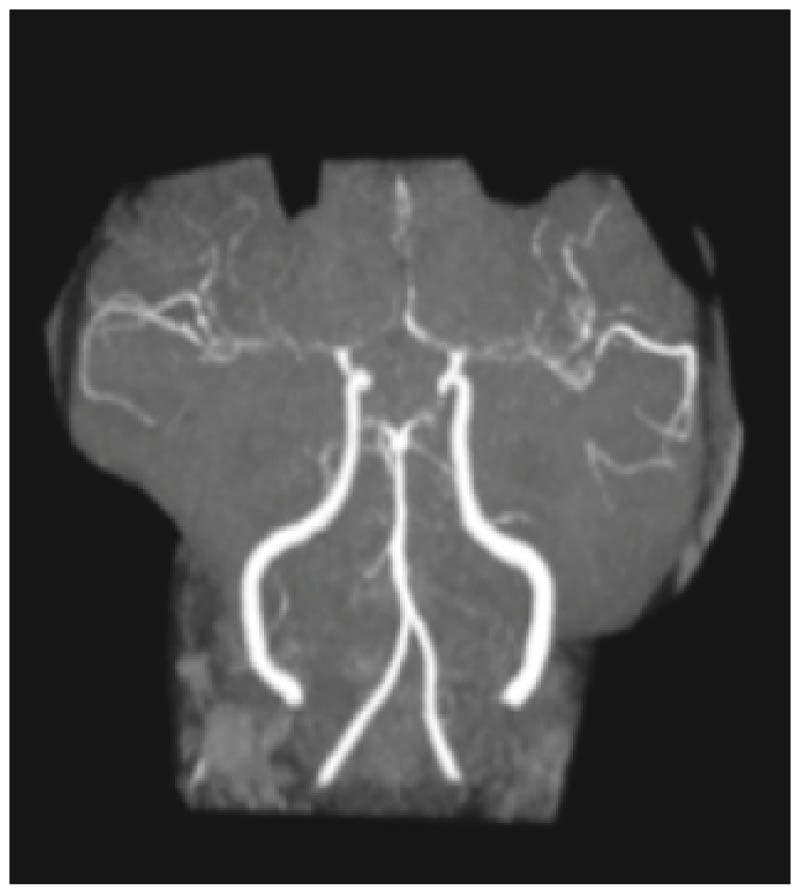
Figure 2A: Non-contrast magnetic resonance angiography of the head.
Time-of-flight magnetic resonance angiography of the circle of Willis reveals diffuse, multifocal segmental narrowing of the circle of Willis involving the anterior cerebral arteries, middle cerebral arteries, and posterior circulation. This is consistent with severe cerebral vasospasm.
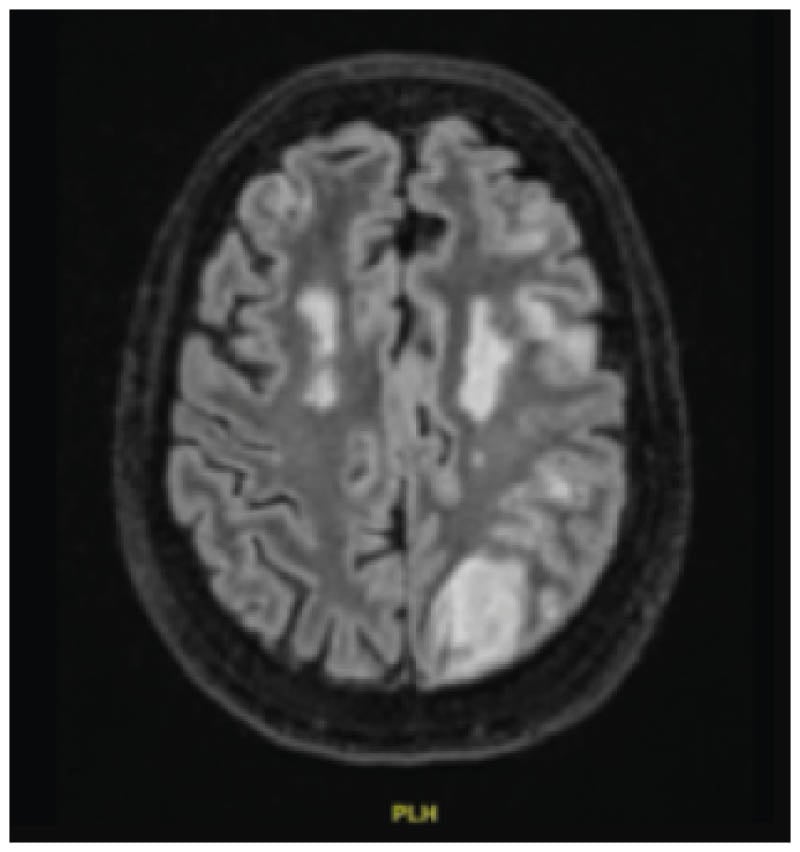
Figure 2B: MRI fluid-attenuated inversion recovery sequence.
Axial fluid-attenuated inversion recovery (FLAIR) MRI sequence shows symmetric, hyperintense lesions in the bilateral frontal lobes, representing subacute infarcts in watershed territories. These findings prompted further investigation for vasculopathy and supported the diagnosis of reversible cerebral vasoconstriction syndrome.
THERAPEUTIC INTERVENTION
The patient was treated with intra-arterial milrinone and verapamil during the cerebral angiography (Figure 3). Pharmacologic therapy was initiated with nimodipine at a dose of 30 mg, four times a day, titrated as needed. In addition, she received supportive therapy, including physiotherapy, occupational therapy, and speech-language pathology services. Corticosteroids were discontinued upon confirmation of RCVS, as they are ineffective for this condition and may lead to worse outcomes in some people.
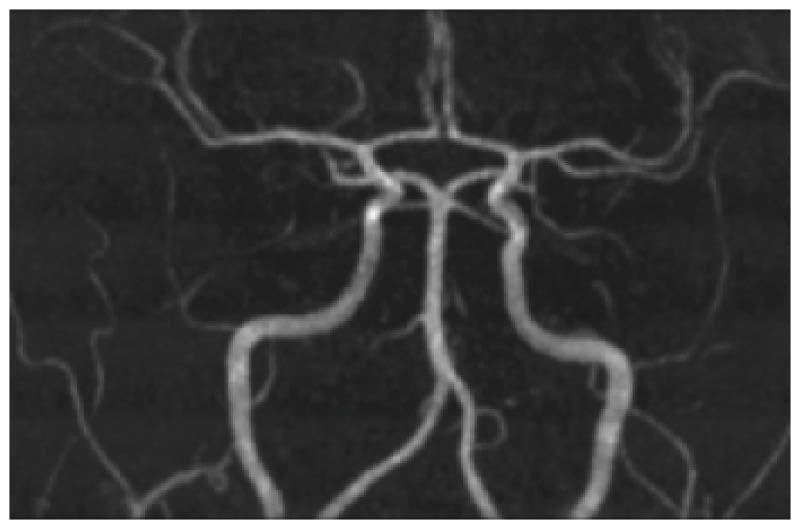
Figure 3: Digital subtraction angiography showing anterior and middle cerebral arteries.
A digital subtraction angiography performed after an intra-arterial administration of milrinone and verapamil. It shows a near-complete resolution of prior segmental vasoconstriction in the anterior and middle cerebral arteries. These findings confirm the reversible nature of the vasospasm, supporting the diagnosis of reversible cerebral vasoconstriction syndrome and ruling out fixed stenotic processes such as vasculitis.
FOLLOW-UP AND OUTCOMES
Following treatment, the patient’s symptoms stabilized, and she showed improvement in cognitive function with the resolution of acute neurological deficits. Rehabilitation services were initiated to address residual deficits. Repeated neuroimaging was planned to monitor vascular status. Given the incidental finding of thyromegaly, thyroid function tests were also performed and were to be followed up as an outpatient in this regard.
The patient demonstrated good adherence to nimodipine therapy, with no significant side effects reported. One notable adverse event was an acute rise in creatinine induced by acyclovir, which was resolved with hydration.
TIMELINE OF CLINICAL EVENTS IN 2024
- Early September: Initial symptoms of confusion and leg weakness.
- Mid-September: Head CT unremarkable.
- Late September: MRI shows multifocal infarcts; empiric antibiotics are given for presumed infection.
- Early October: Cerebral angiography confirms reversible cerebral vasoconstriction syndrome; intra-arterial therapy given.
- Mid-October: Initiation of nimodipine and rehabilitation services.
- Late October: Clinical stabilization; discharged with outpatient follow-up.
DISCUSSION
This case highlights the value of a cerebral angiography in differentiating RCVS from similar conditions.4,5 Limitations included the delayed access to neurointerventional studies, and psychosocial barriers.6,7 Cannabis use has been associated with RCVS in several case series and reviews, potentially through the modulation of cerebral vascular tone. Given the patient’s daily cannabis use, it may have been a precipitating or exacerbating factor in this case.8
RCVS is often underdiagnosed as it masquerades as vasculitis and other cerebrovascular disorders.9,10 Acute management with calcium channel blockers has been shown to be useful, as demonstrated in the present case, as the reversibility of vasospasm that is evidenced by intra-arterial therapy is diagnostic of RCVS and warrants targeted treatment with nimodipine.11-14 Although calcium channel blockers such as nimodipine are the mainstay of treatment, other agents like magnesium sulfate have been trialed with varying success.15 However, evidence remains limited. Patients with RCVS typically have a good long-term prognosis with the resolution of vasoconstriction, though some may develop residual deficits or recurrent events. It is advised to monitor for complications such as seizures, posterior reversible encephalopathy syndrome, and stroke recurrence.16
PRIMARY TAKEAWAY
RCVS must be included in the differential diagnosis of patients with multifocal infarcts of unclear etiology, as early diagnosis and treatment can greatly influence outcomes.17







