Written by Dr Inna Lutsenko and Ms Aishoola Sultanova, on behalf of the European Stroke Organisation (ESO)-EAST, Kyrgyzstan
![]()
The 5th International Symposium on Collaterals to the Brain (Collaterals 2018) took place on 6–8th November 2018 in Los Angeles, California, USA. This global conference was organised by Prof David S. Liebeskind and Prof Ashfaq Shuaib. Prof Liebeskind is the Director of the Neurovascular Imaging Research Core, Associate Director of the UCLA Stroke Center, Director of Outpatient Stroke and Neurovascular Programs, Los Angeles, California, USA, and Prof Ashfaq Shuaib is a Professor in the Division of Neurology, Faculty of Medicine and Dentistry, University of Alberta, Canada; Head of Neurosciences Center and Department of Medicine Hamad Medical Corporation, Doha, Qatar.
The University of California, Los Angeles (UCLA), California, USA is a member of the prestigious international Universities Research Association group, and the University’s School of Medicine is one of the university’s most highly ranked graduate schools.1 Furthermore, The UCLA Stroke Center has been recognised as one of the world’s leading centres for the management of cerebral vascular disease by the Joint Commission and the American Heart Association/American Stroke Association (AHA/ASA).2 The International Symposium on Collaterals to the Brain has been held annually since 2012, when the first symposium brought together 30 experts and 200 participants.3 This year the conference brought together >50 invited experts from around the world to connect with representatives from >50 countries and regions via the live webinar and interactive broadcast from Los Angeles.
The symposium consisted of 24 sequential, 40-minute sessions led by different countries from around the world. Country representatives, practical neurologists, and neurosurgeons shared their research findings via teleconference, and their presentations were visible for all conference participants. The interactive broadcast from Los Angeles lasted for 2 days from early morning to late night and provided global access to >50 presentations from >50 countries.
The first day of the conference was the7th November, which gave several prominent speakers and researchers the opportunity to present their fascinating findings. Dr Roni Eichel, Director of the Stroke Unit and Neurological ICU in Jerusalem, Israel, shared in his presentation ‘Fast Stroke Track: The Jerusalem Model’, which detailed how the stroke society in Jerusalem is increasing the awareness of the city’s population about stroke and its consequences by creating of a FAST (Facial drooping, Arm weakness, Speech difficulty, Time to call emergency services) algorithm in the national languages.
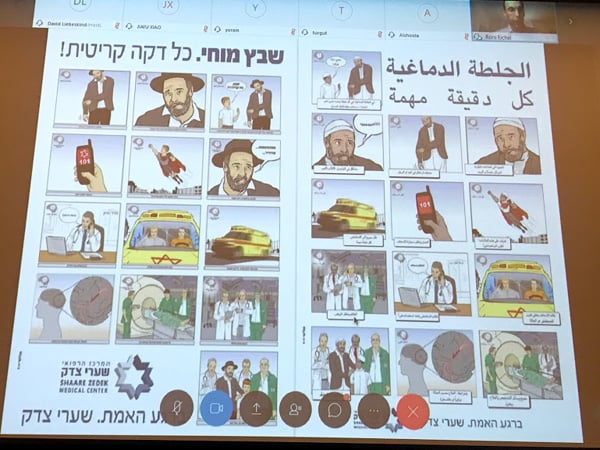
The FAST algorithm poster displayed in Hebrew (left) and Arabic (right).
Prof Jan Claude Baron (France) shared his findings that focussed on discovering which patients are most likely to benefit from thrombolytic treatment. They used retrospective analysis of six registries, with inclusion criteria of acute ischaemic stroke patients treated with intravenous thrombolysis (IVT). A collaterals flow map was demonstrated on 6 slices and in 3 phases (early, mid, and late). The research found that a predictor of post-IVT early recanalisation is thrombus <1 mm in size (odds ratio: 0.67). French neurologists announced that there is an independent association between collaterals and early recanalisation showing that with better collaterals there is more chance to have early IVT recanalisation before thrombectomy. This finding is consistent with the hypothesis that delivery of thrombolytic agents to both ends of the thrombus may enhance early recanalisation.⁶
Dr Vincent Costalat (France) presented his study ‘Ischemic Stroke treatment. The next Frontier’. Dr Costalat directed attention to a special group of patients that have a National Institutes of Health Stroke Scale (NIHSS) score of 0 or a low score with large vessel occlusion (LVO). He gave the clinical example of a 74-year-old patient with total left hemiparesis, who developed a total recovery (NIHSS 0). In his treatment, no fibrinolisis and no anticoagulants were used. After 3 months, the patient’s modified Rankin Scale score was 2 and he developed cognitive impairment. In patients with LVO with diffusion-weighted imaging positive infarcts, even a status of NIHSS 0 can lead to serious consequences. Many patients have silent infarctions and a very low NIHSS score despite of the large size of the fresh infarction. The patient’s condition could be explained by the length and quality of collaterals, but even in a very good collateral system the thrombus will resolve itself until the collaterals are exhausted. Dr Costalat presented the ongoing MOSTE study, which is an international, multicentre, prospectively randomised to two parallel (1:1) arm, open treatment, blinded endpointed (PROBE) trial. The goal of the study is to demonstrate the superiority of mechanical thrombectomy associated with best medical therapy (BMT) compared to BMT alone for the increase in the functional independence of patients with LVO harbouring minor stroke symptoms (NIHSS score <6). Based on the study, the ‘Registry for perfusion data prospectively collected for sub analysis’ was organised.
Dr Simone Beretta from the laboratory of Experimental Stroke Research, School of Medicine, University of Milano Bicocca and Milan Center for Neuroscience (NeuroMi), Milano, Italy presented his study focussing on the correct positioning of the head during an acute period of stroke. Dr Beretta’s presentation ‘Safety of Head Down Tilt 15° (HDT15°) in experimental intracerebral haemorrhage: Relevance for gravity-based modulation of collaterals in acute stroke’ underlined the effectiveness and safety of keeping the head of the patient tilted down on 15o after a stroke, thereby improving the patient’s condition.
The highlight of the day was the presentation ‘Stroke and Hypertension’ by Prof Marilyn Cipolla from Burlington, Vermont, USA. Prof Cipolla underlined that hypertension increases the volume of cerebral infarction, worsens outcomes after a stroke, and reduces penumbra.
Dr Andrey V Alexandrov (Australia) moderated the session from Russia and Kazakhstan. An interesting presentation was made by Dr Dmitriy Kislitsin, Dr Anton Gorbatyh, and Dr Kirill Orlov from the Interventional Neuroradiology and Neurosurgery department, Novosibirsk, Russia. In large arteriovenous malformations (AVM), there is a risk of a blood pressure dropping after the AVM’s removal. Since 2013, the dual sensor doppler guidewire has been used to measure flow and pressure in feeding vessels and draining veins of specific AVM. The action of this device was demonstrated by Russian neurosurgeons. Dr Alexandrov noted: “in the zone of AVM, blood vessels around the whole area ‘do not know’ how to regulate, the new bloodflow is diverted, intravascular pressure is specially adjusted to the malformation, and its sudden removal could lead to an unadjusted breakthrough of collateral circulation. If you drop the velocity below 30%, you critically drop cerebral bloodflow.”
Additionally, there were presentations from Kyrgyzstan and Tajikistan. European Stroke Organisation (ESO)-EAST-Kyrgyzstan co-ordinator Dr Inna Lutsenko was invited in person to moderate the Central Asian session. Dr Lutsenko shared her research findings in her presentation titled ‘Clinical and etiopathogenetic features of patients during the ischemic stroke according to TOAST classification: Data from SITS-Kyrgyzstan stroke registry’ In her speech, Dr Lutsenko presented information on the prevalence and logistics of stroke in Kyrgyzstan and indicators of the severity of a patient’s condition after a stroke at different altitudes above the sea level, based on the results of the SITS and RES-Q stroke registries. Dr Lutsenko presented the “onset-to-door time” in Kyrgyzstan, which is prolonged compared to some other countries. Due to the lack of facilities in remote areas, patients are admitted late to the clinic, thereby missing the golden hours for thrombolysis. Now, a big educational campaign for patients is underway, based on the FAST algorhythm (which is now translated into Kyrgyz), educational speeches, and events lead by volunteers of ESO-EAST in Kyrgyzstan for patients and their relatives. Chief Neurologist of Bishkek, Kyrgyzstan, Dr Abdusalim Artykbaev, the head of the Vascular Neurology Department of Bishkek City Civil Clinic Number 1, made a remote presentation about the stroke statistics in Bishkek and the prevalence of ischaemic stroke in this regions. Dr Artykbaev mentioned the achievements of ESO-EAST in Kyrgyzstan, such as optimising working with the RES-Q and SITS registries and the involvement of new clinics from rural regions in registries.

The symposium continued on the 8th of November. Dr Marios Psychogios (Germany) made a noteworthy presentation on multiphase flat-detector computed tomography angiography (mpFDCTA) imaging. The conclusions of the presentation were that mpFDCTA imaging provides evaluation of the collaterals prior to digital subtraction angiography, leading to door-to-reperfusion times of ~60–70 minutes and improving the clinical outcomes of the patients with LVO.
The highlight of the day was the speech of Prof Dr Urs Fischer, University Hospital (Inselspital), Secretary General of the ESO, Bern, Switzerland. Prof Fischer made the conclusion that treatment with intravenous tissue-type plasminogen activator before thrombectomy did not seem to affect the occurence of infarcts in new territories and infarcts in initially new territory, thus warranting further research on associated factors.
A further highlight was the speech by Prof Dr Werner Hacke, Heidelberg University, Heidelberg, Germany, and the Immediate Past President of the World Stroke Organisation.
The presentation by Prof Hacke detailed a a complete database of patients with access to mechanical thrombectomy in Germany. Dr Prof Hacke stated: “in Germany, everyone had access to thrombectomy […] but not everyone who was eligible was commonly treated. This was a good start. There were about 400 stroke centres and only 180 of them had fulfilled the criteria of having new care, new surgery, vascular surgery on site, and interventional [capabilities] on site. Our initiative needed effort and it needed a long-term planning for stroke services beyond thrombectomy alone.” Prof Hacke also noted that there is a lack of neurologists and stroke should be treated by only specialist neurologists.
The words of Dr Prof Hacke were supported by the representative of Japan, Prof Noboyuki Sakai, who explained that there are about 1,400 specialised neurologists in Japan who are able to perform thrombectomy.
Dr Simon de Meyer, Laboratory of Thrombosis Research, Leuven, Belgium presented ’Novel targets for thrombolysis in ischemic stroke’. He presented the large spectrum of different sizes of thrombus and noted that the ‘one size fits all rule’ does not work in this case and the size of the thrombus influences its dilution during the thrombolysis process. Dr de Meyer underlined that von Willebrand Factor is a new thrombolytic target in ischaemic stroke.
Dr Ivo Jansen (Netherlands) gave a presentation titled ‘Collaterals in Routine Stroke Practice: Results from Mr Clean Registry’ on behalf of the Mr Clean investigators. Additionally, Dr Jansen, together with collaborator Mr Renan Sales Barros, the Chief Technology Officer at NicoLab, Amsterdam, Netherlands, presented their work from NicoLab. NicoLab presented StrokeViewer, which offers physicians clinical decision support through complete assessment and remote viewing of relevant imaging biomarkers within 3 minutes. Algorithms were developed using artificial intelligence, allowing high accuracy and fast analysis of relevant biomarkers from stroke imaging (non-contrast CT, CTA, dynamic CTA, and follow-up imaging).5
Prof Sheila Martins, Medical School, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil presented date from the RESILENT trial. The objective of this trial was to evaluate the hypothesis that mechanical thrombectomy with the stent retriever and or thromboaspiration is superior to medical management alone in achieving more favourable outcomes in the distribution of the modified Rankin Scale scores at 90 days in subjects presenting with acute large vessel ischaemic stroke in anterior circulation ≤8 hours from symptom onset in public hospitals in Brazil.
Dr Alan Flores, San Lorenzo, Paraguay moderated the session from Argentina, Chile, and Paraguay. He gave a presentation on the impact of pre-hospital stroke code in a public centre in Paraguay; it was an observational, single-centre study, which took 3 years of experience in reperfusion treatment.

Collaterals 2018 was very successful, as in previous years, and proved once again that this type of innovative and unique conference provides an opportunity for neurologists and neurosurgeons from different parts of the world to share their research with colleagues from other countries, even presenting remotely. The Collaterals symposium is also a great platform for neurologists all over the world to discuss the main problems in acute stroke treatment in their countries. Due to the remote presence available at Collaterals 2018 and innovative live broadcasting, it was possible for young scientists from developing countries to audit the speeches of prominent stroke researchers and learn a lot in the field of mechanical thrombectomy, early thrombolysis invention, and studies on brain collaterals. This unique forum of expertise emphasised the timely impact of collaterals on a monumental scale, encouraging maximal participation, rapid diffusion, and added value of diverse networking.4
Collaterals 2018 was endorsed by European Stroke Organisation among many other endorsements.
References
- Site US news. Available at: https://www.usnews.com/education/best-global-universities/university-of-california-los-angeles-110662. Last accessed: 7 January 2019.
- Site UCLA Newsroom. Available at: http://newsroom.ucla.edu/releases/ucla-stroke-center-awarded-comprehensive-244035. Last accessed: 7 January 2019.
- Site Grantome. Available at: http://grantome.com/grant/NIH/R13-NS082049-01. Last accessed: 7 January 2019.
- Liebeskind DS et al. Collaterals 2016: Translating the collaterome around the globe. Int J Stroke. 2017;12(4):338-42.
- Site NicoLab. Available at: https://www.nico-lab.com/wp-content/uploads/StrokeViewer_flyer-1.pdf. Last accessed: 7 January 2019.
- Bang O. Y. et al. Collateral Circulation in Ischemic Stroke: Assessment Tools and Therapeutic Strategies. Stroke. 2015 Nov; 46(11): 3302–3309.
- Site The National Center for Biotechnology Information (NCBI). Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624512/. Last accessed: 9 January 2019.








