Abstract
Branchial cysts appear most often as unilateral neck masses and account for 25% of head and neck congenital swellings, of which 95% arise from the second branchial cleft. Here, the authors report a rare case of branchial cleft cyst in a 16-year-old girl, which is often misdiagnosed and treated improperly.
INTRODUCTION
The branchial cleft’s embryological journey begins between the first 3–8 weeks of intrauterine life. Five mesodermal arches form by the inpouching of ectodermal clefts and endodermal pouches; however, incomplete obliteration of these clefts result in anomalies such as cervical lymphoepithelial cysts, branchial cysts, sinus tracts, or fistulae.1,2 The occurrence of branchial cleft cysts shows no significant gender predilection and presents in young adults with peak incidence during the third decade of life.2-4 Branchial cysts appear most often as unilateral neck masses and account for 25% of head and neck congenital swellings, of which 95% arise from the second branchial cleft.4
CASE REPORT
A 16-year-old girl reported to the hospital with a swelling in the right side of the neck which was present from childhood and was slowly increasing in size. Her medical history was insignificant. On clinical examination there was 5×4 cm round swelling in the right side of the neck below the sternomastoid muscle, and was non-tender, non-pulsatile, fluctuant, and soft in consistency (Figure 1). There were no associated complaints such as pain, change in voice, or difficulty in breathing. The swelling was not moving with protrusion of tongue or on deglutition, and there was no history of discharge during eating or drinking. A clinical diagnosis of congenital cyst or paraganglioma was made. Pre-operative haematological investigations were carried out and were within normal limits. Ultrasonography (US) guided fine needle aspiration cytology (FNAC) revealed a milky, white-coloured fluid which was confirmed as a branchial cleft cyst. A contrast MRI was performed to find the extent of the cyst and its relation to the internal jugular vein and carotid artery (Figure 2). Surgical removal was planned, and a submandibular incision was directed to the right side of the neck. Dissection was performed carefully to avoid puncture of the cyst. The cyst was detached from the base and enucleation was completed (Figure 3). All the major vessels and cranial nerves were saved. The final histopathological report confirmed the swelling as a branchial cleft cyst. Drain number 12 was kept and closure was completed in layers.

Figure 1: 5×4 cm round swelling in right side of the neck below the sternomastoid muscle, non-tender, fluctuant, and soft in consistency.
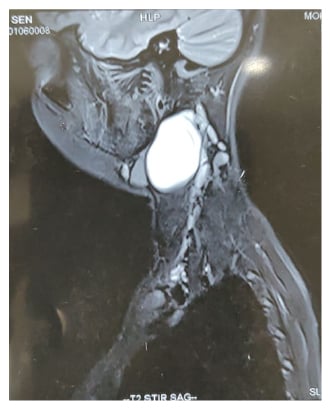
Figure 2: MRI with contrast was carried out to find the extent of the cyst and its relation to the internal jugular vein and carotid artery.

Figure 3: The cyst was detached from the base and enucleation was complete. All vital neuro-vascular structures were saved.
DISCUSSION
The earliest report of a branchial cyst was by Hunczovsky in 1785.1 These cysts are common but often present diagnostic dilemmas to clinicians and radiologists and challenge surgeons because of the close anatomical presence to vital neurovascular elements. It has become imperative to document each variation and occurrence of these cysts closely to develop a protocol and strategy for effective management.5-7
Understanding of the pathophysiology of these cysts is paramount to understanding them as an entity. Various theories have been proposed to explain the origin of branchial cysts, including their consideration as epithelial inclusions within a lymph node, or alternatively as remnants of an original connection between the thymus and third branchial pouch. Other theories include the cervical sinus theory and the branchial apparatus theory. The cervical sinus theory suggests the origin of these cysts is from the remains of the cervical sinus of His, formed by the growing down of the second arch and its fusion with the fifth arch. Conversely, the branchial apparatus theory states that the origin is routed in pharyngeal pouches or branchial clefts.8-10 This case is rare in the authors’ surgical setting and here the detailed sequence of its management is reported.
MANAGEMENT OF BRANCHIAL CLEFT CYST
Evaluating a patient suspected with having a branchial cleft will involve a conglomeration of clinical examination and imaging modalities. The clinical and most commonly diagnostic signs include a slow progressing mass that can be present from weeks to years with overlying normal skin. Palpation reveals smooth, round, soft, non-tender, fluctuant, mobile, and asymptomatic masses. These cysts rarely have potential for malignant transformation and rupture. Primary branchial cleft cyst is typically located between the external auditory canal and submandibular area and it is usually in close proximity to the parotid gland and facial nerve.10,11 It has two types of presentation; Type 1 is characterised by duplication of the membranous external auditory canal; and Type 2 is composed of ectomesoderm and cartilage. The clinical presentation is usually soft tissue mass or draining sinus in the retromandibular region accompanied by ear discharge. Secondary brachial cleft cysts lie between the lower anterior border of the sternocleidomastoid and the tonsillar fossa, close to the glossopharyngeal and hypoglossal nerve, and carotid vessels. They become tender if secondarily inflamed or infected. Inspect for mucoid or purulent discharge on the skin or into the pharynx via draining sinus tracts.12
The authors relied on initial fine needle aspiration to distinguish a cleft cyst from malignancy when carrying out radiographic assessment. Contrast enhanced CT, US, and, MRI also significantly contributed to arriving at a preoperative diagnosis and treatment trajectory. Odontogenic infection, cystic hygroma, enlarged lymph nodes, paragangliomas of the vagus nerve, lipoma, carotid body tumours, neurofibroma, haemangioma, lymphangioma, teratoma, ectopic salivary tissue, pharyngeal diverticulum, laryngocele, saccule, and cystic schwannoma13 should be ruled out as they constitute the differential diagnostic possibilities of a branchial cleft cyst.14 Elective excision is the most
favourable treatment for a branchial cleft cyst because of the risk of infection, further enlargement, or malignancy. Aesthetic concerns entail the use of a transverse incision directly over the cyst. Care should be taken to avoid important vascular structures such as the internal and external carotid arteries, and nerves like the superior laryngeal, glossopharyngeal, vagus, and hypoglossal nerve. Surgical complications arise occasionally, and one must be prepared to manage events like recurrence, persistent fistula, and damage to the cranial nerves.12
CONCLUSION
Effective management of branchial cleft cysts predominantly rests on surgical precision which improves with proper understanding of the entity coupled with good radiographic assistance. As branchial cleft cyst has many differential diagnoses, it is important to confirm the diagnosis by histopathological examination of the excised tissue.13








