Abstract
The occurrence of bladder outlet obstruction (BOO) in men with prostate cancer is common. Although relieving the obstruction may not change prognosis, it is highly valued by patients and is generally associated with improvement in general functioning and wellbeing in the short-term. The aim of this study was to assess the efficacy of high-dose external beam radiation therapy (EBRT) combined with bilateral subcapsular orchidectomy (BSO) to relieve BOO due to prostate cancer.
A retrospective study design was employed and conducted at the Mulago National Referral Hospital. Records of all patients with high-risk prostate cancer who presented with urinary obstructive symptoms and treated with the BSO and EBRT were retrieved. The study variables were age, clinical stage, and pathological Gleason score. The endpoint of the study was for patients to be able to pass urine after removing the urethral catheter, analysed as follows: complete failure to pass urine; partial emptying with a post-void volume >100 mL, and passing urine with complete emptying and a post-void volume <100 mL.
In total, 46 patients were analysed in the period of January 2011–December 2012. Mean age was 71 years (range: 63–93). Eight patients failed to pass urine, while six passed urine incompletely (partial emptying). Thirty-two passed urine with a good stream and emptied the bladder completely. The success rate was 32/46 (70%). All patients had T3 and T4 stage disease with Gleason scores >8. In conclusion, orchidectomy combined with EBRT was found to be an effective and feasible option for relieving BOO due to prostate cancer.
INTRODUCTION
Non-communicable diseases, including cancers, are becoming increasingly important as causes of morbidity and mortality in Sub-Saharan Africa, including Uganda. Cancer of the prostate is the most common malignancy in males in Uganda.1 It is most prevalent in the sixth and seventh decades of life, as it is elsewhere in the world.2 Bladder outlet obstruction (BOO) is a common presentation in men with high-risk prostate cancer.3 Whereas the prevalence of advanced and metastatic disease is reduced in high-income countries, this is not the case in low-income countries, especially in Sub-Saharan Africa, where cancer screening services are almost non-existent and access to cancer treatment is limited.4
Immediate relief is usually obtained by either suprapubic catheter or an indwelling urethral catheter.5 Prolonged catheterisation has a major impact on quality of life (QoL) in addition to the risk of urinary tract infections.5-7 Definitive treatment of the obstruction, according to the standard practice pattern in many countries, is a channel transurethral resection of the prostate (TURP).8 Some concerns have been raised about channel TURP and these include intractable postoperative bleeding, prostatorectal fistula, and re-obstruction due to regrowth of the tumour.9
There is evidence that urinary obstruction caused by prostate cancer can be relieved by irradiation, however the results of combining radiotherapy and orchidectomy have not been assessed.10 Given the decreasing incidence of BOO due to prostate cancer in general, this applies mostly to middle and high-income countries. Only a few articles have been published recently on obstructive uropathy from prostate cancer.11
This study reports relief of BOO from a combination of bilateral subcapsular orchidectomy (BSO) and external beam radiation therapy (EBRT) in a resource-limited setting.
METHODS
Design
This was a retrospective descriptive study.
Setting
This work was conducted at an urban teaching hospital in Kampala, Uganda: a Sub-Saharan Africa resource-limited environment. The Mulago National Referral Hospital is a 1,500 bed hospital with numerous subspecialised units, including urological services, which are largely provided free of charge in this public hospital.
Eligibility
Records of all patients with BOO, as a result of high-risk prostate cancer, who had attended the urology clinic between 4th January 2011 and 31st December 2012, were retrieved and reviewed. A list generated from the operating theatre log of patients who had undergone BSO was used to retrieve the patient files from the records department archives.
The diagnosis of cancer had been proven by histological diagnosis after findings of raised prostate surface antigen (PSA) and digital rectal examination that revealed locally advanced disease. BOO was defined as a self-reported situation when a patient diagnosed with prostate cancer could not void urine partially or completely.
Conventional External Beam Radiation Therapy
Two weeks after BSO, EBRT was delivered by means of a two-field technique. The fields were antero-posterior, postero-anterior, and were designed to include the prostate, the seminal vesicles, and the regional lymphatic channels. EBRT was delivered in 10–15 fractions to a total dose of 35–45 Gy. Two weeks after irradiation, the catheter was removed.
Study Variables
The main outcome measure was the ability to pass urine through the urethra. Other variables such as haematoma, bladder stones, and hydronephrosis were not captured.
Those who reported passing urine satisfactorily underwent an ultrasound examination to assess the post-void residual urine volume. A volume >100 mL was considered significant and indicative of incomplete emptying, and therefore considered as treatment failure. Age, Gleason score, and clinical stage were the other study variables considered.
Ethical Considerations
All patients provided written informed consent for all the procedures that were done. Clearance was obtained from the Mulago Hospital Ethics and Research Review Board.
RESULTS
A total of 46 patients were included in the study analysis. The mean age was 71 years with a range between 63 and 93 years. The median follow-up period was 9 months and the range was 6–12 months.
The final outcome measures were as follows: 32 individuals (70%) reported passing urine satisfactorily and had post-void volumes <100 mL while 5 patients (9%) failed to pass urine at all; the remaining 9 patients (11%) were able to pass urine only partially with post-void volumes >100 mL (Table 1). All prostate specimens had pathological Gleason scores ≥8. The stage was T3 or T4. The patients who failed to pass urine had their urethral catheters reinserted.
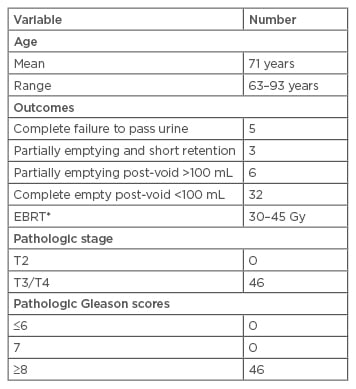
Table 1: Age and study outcomes: Palliative Radiotherapy and Hormonal Deprivation Ugandan Study for Prostate Cancer 2015.
EBRT: external beam radiation therapy.
*EBRT in 10–15 fractions.
DISCUSSION
The study set out to investigate the efficacy of BSO and EBRT in relieving BOO in patients with locally advanced prostate cancer in a resource-limited setting. Assessment was limited to ease or completeness of passage of urine. Results showed that 70% of patients were able to satisfactorily pass urine during the follow-up period (which lasted at least 6 months), a similar outcome to several other studies where a high radiation dose was administered.12,13 Although numerous studies highlight the treatments of early and advanced stage prostate cancer and its complications, there is a paucity of studies specifically investigating androgen deprivation and EBRT for BOO due to prostate cancer,14 especially in resource-limited environments.
It is important to relieve urinary obstruction as it generally improves QoL;5-7 long-term effects depend on the severity of the blockage, its acuity, laterality, and the patient’s underlying renal function. Obstructive uropathy from prostate cancer most commonly results from bilateral ureteral blockage or unilateral ureteral obstruction in the setting of a solitary renal unit.11,15 Obstruction has a deleterious impact on tubular function with diminished urinary concentrating ability, which, if left uncorrected, leads to further interstitial inflammation and ultimately fibrosis.15 Long-standing (>6 weeks) obstruction may not yield much functional benefit, a factor we take into account when making treatment decisions.11,15
The diagnosis of obstructive uropathy is made by history and physical examination, often worsening obstructive voiding symptoms are also used, and in some cases acute urinary retention. Urea and electrolyte levels and imaging can confirm renal insufficiency. In practice, contrast imaging is normally avoided to prevent contrast induced nephropathy, which further impairs renal function.15
In this series, management was directed to relieving BOO after physiological derangements were corrected to optimise outcomes.16,17 Initial relief was obtained by inserting a Foley’s catheter and the other relief options were EBRT and BSO.
High-dose EBRT slows down biochemical or clinical progression, more so than a conventional-dose radiation, but no EBRT regimen, whether conventional, high-dose conformal, dose fractionated, or hypofractionated, is superior in reducing androgen deprivation to decrease overall disease-specific mortality. In resource-limited settings such as this, the availability of stents or palliative TURP is limited or non-existent.
STUDY LIMITATIONS
Combination therapy was used, which makes it difficult to delineate which modality had a preferable efficacy and to what extent each therapy contributed to the patient outcome. Though we know radiation is slower than endocrine therapy in diminishing prostate cancer biomarker PSA,18 this does not conclusively delineate the contribution of each modality. The study design was retrospective and may not bring out the other variables of QoL assessment. Uroflowmetric measurements were not taken due to resource limitations.
CONCLUSION
BSO combined with high-dose palliative EBRT was effective in relieving BOO in high-risk prostate cancer patients. It is an alternative to the often unavailable channel TURP procedure or permanent indwelling suprapubic or urethral catheter drainage among men in resource-limited settings.








