Abstract
Schwannomas are neurogenic, benign, slow growing tumours that originate in Schwann’s intersecting fascicles of the peripheral nerves. This article reports the case of a previously healthy 51-year-old male, where a 9.0×6.5 cm (3.5×2.5 in) sized pleural mass was found after the patient presented a haemoglobin level of 3.2 g/dL in a blood smear at a routine check-up. The patient had no relevant medical, family, or psychosocial history and presented no relevant symptoms.
After diagnosing and treating a chronic haemorrhoidal disease, the tumour was removed and studied. Demonstrating histopathological and immunohistochemical features of schwannoma, its uniqueness and rarity after successful management of the disease contributes to the medical literature as a histopathologic diagnostic standard and a therapeutic option for future cases of pleural schwannoma.
Sharing the histopathologic features of schwannoma is not common, usually, the available case reports are lacking. The patient was able to recover fully and had no significant or severe complications associated with medical care.
![]()
Erratum: Primary Pleural Schwannoma as Incidental Findings: An Unusual Case Report
Authors: Marcos Cherem-Kibrit, Elias Zonana-Schatz, Crisitina Alvarado-Silva
Original citation: EMJ Oncol. 2022; DOI/10.33590/emjoncol/21-00267. https://doi.org/10.33590/emjoncol/21-00267.
Date correction published: 27.10.2022
In the article by Cherem-Kibrit et al., published in EMJ Oncology on 23.05.22, the following figure title was incorrect: “Figure 1: Schwannoma during the minimally invasive surgery before converting it to an open thoracotomy.” The title should have read: “Figure 1: Axial and coronal IV contrast, enhanced high resolution chest CT scan.” This has now been corrected.
EMJ apologises for the error and any inconvenience caused.
![]()
Key Points
1. A schwannoma is a slow-growing, neurogenic, and benign tumour, which originates within the peripheral nerves, on Schwann’s intersecting fascicles. They are usually located in the head, neck, and flexor surfaces of the extremities; this case reports a rare case of a pleural schwannoma.2. Histopathologic reporting of schwannomas notes microscopic Antoni A and B areas in most cases of pleural schwannoma, where Antoni A shows areas of hyper-cellularity with Verocay bodies, and Antoni B represents areas of myxoid hypocellularity exhibiting degenerating changes such as cystic formation, calcification, haemorrhage, xanthomatous infiltration, and hyalinisation.
3. Histopathologic diagnosis should be standard practice, as the histologic differential diagnosis includes spindle cell tumours, such as neurofibroma, leiomyoma, leiomyosarcoma, and calcifying aponeurotic fibroma.
INTRODUCTION
Schwannomas are neurogenic, benign, slow growing tumours that originate in Schwann’s intersecting fascicles of the peripheral nerves. Usually, schwannomas are located in the head, neck, and flexor surfaces of the extremities. They are not usually located in the mediastinum and retroperitoneum. Most intrathoracic neurogenic tumours originate in the posterior mediastinum and only 5.4% are in the chest wall.1
Approximately 95% of the pleural dependent tumours are malignant, most of which present as a product of metastasis. Needless to say, benign pleural tumours are very unusual and, among them, schwannoma is much less frequent.2
To the best of the author’s knowledge, around 20 pleural schwannoma cases have been reported in the medical literature to date.
Herein, this article reports the case of a previously healthy 51-year-old male where a 9.0×6.5 cm (3.5×2.5 in) sized pleural mass was found after the patient presented with a haemoglobin (Hb) level of 3.2 in blood smear at a routine check-up. The tumour was removed and studied. Demonstrating histopathological and immunohistochemical features of schwannoma, its uniqueness and rarity after successful management may contribute to the medical literature as a histopathologic diagnostic standard and a therapeutic option for future cases of pleural schwannoma.
CASE REPORT
A previously healthy 51-year-old male, with no relevant medical, family, and psychosocial history, presented at the emergency room asymptomatic due to a 3.8 g/dL Hb laboratory finding in their routine check-up. They had been a smoker for 20 years, with a Global Tobacco Index score of 5 packs/year and no history of asbestos exposure, thoracic radiation, or recent trauma. During discussions with the patient, a history of haemorrhoidal disease was identified, consisting in chronic anal bleeding. The patient achieved haemodynamic stabilisation after the Hb results, and a blood pack transfusion was performed. After a series of transfusion protocols over several days, a 10 g/dL haemoglobin level was achieved.
During the routinary haemorrhoidectomy pre-operation exams, anterior-posterior and lateral chest X-rays showed an unexpected 9.0×6.5 cm (3.5×2.5 in) round-like, radiopaque mass in the right chest wall, between the middle and the superior lobe, which needed further study. The authors decided that a thoracoabdominal CT scan was needed in order to evaluate the extension. The study showed a round, encapsulated 10.0×6.5 cm (4.0×2.5 in) and hypodense pleural mass in the right posterosuperior hemithorax, which was full of liquid content, with probable infiltration to the third rib, in intimate contact with the parietal pleura (Figure 1).

Figure 1: Axial and coronal IV contrast, enhanced high resolution chest CT scan.
A haemorrhoidectomy was performed without any complications. While the patient was recovering from the procedure, the unknown pleural mass was being held by the thoracic surgery and the medical oncology units for evaluation. Based on imaging characteristics and frequent epidemiological pleural tumours, multiple different diagnoses were considered, including a variety of benign and malignant neoplasms. After another transfusion protocol, which continued elevating the patients’ Hb levels up to 12 mg/dL, the patient was offered a right thoracic exploration using minimally invasive techniques, which they accepted in the following days.
MANAGEMENT AND OUTCOME
In the minimally invasive right thoracic exploration, a 10 cm pleural tumour was observed in the right apex, which was adhered to the upper lobe and to the thoracic wall (Figure 2). Dissection of the lung parenchyma tumour was initiated, and it started to present diffuse bleeding, so a conversion to a right anterior thoracotomy was performed as a result of the lack of visibility. Due to the adherence of the tumour to the pulmonary parenchyma, a non-anatomical segmentectomy of the right lobe was performed.
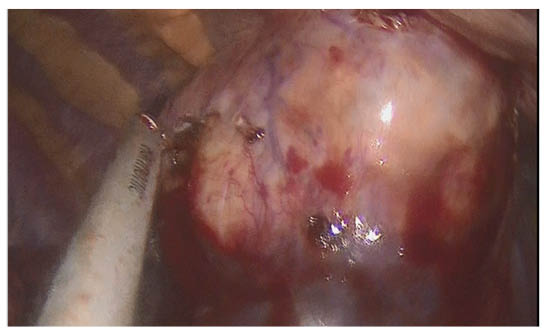
Figure 2: Schwannoma during the minimally invasive surgery before converting it to an open thoracotomy
A specimen was sent for an intraoperative study, discarding a solitary fibrous tumour and a synovial sarcoma, while reporting a solitary pleural fibroma. After the intraoperative pathology reported a lack of malignancy information, the lung parenchyma was confronted and an endopleural tube was placed before closing.
After the surgery, the patient stayed in the intensive care unit for 2 nights, with the intention to keep close monitoring. They presented a satisfactory evolution and control chest X-rays were taken 72 hours after the procedure, which showed a complete lung re-expansion. The patient was discharged from the intensive care unit and was transferred to the internal medicine ward.
The final pathology report arrived a couple of days later and stated the macroscopic gross findings: it was fresh and partially open; it weighed 118 g and measured 10.0×7.5×6.5 cm; it was ovoid, reddish, and smooth; when it was cut, it was a cystic solid, greyish–white and haemorrhagic, with a soft consistency. The immunophenotype was compatible with schwannoma, with a low cellular replication (Ki-67: <1%) and was negative for malignant neoplasia. The microscopic appearance of the haematoxylin and eosin-stained resected tumour images can be seen in Figure 3.
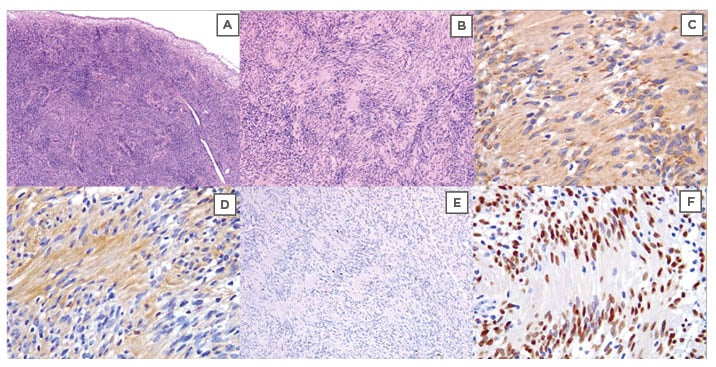
Figure 3: Microscopic appearance of haematoxylin and eosin stained resected tumour.
A and B) Variable orientated cells, which in places appears to be arranged in intersecting fascicles. Cells show a mild degree of variation in nuclear hyperchromasia, mild nuclear pleomorphism, and mild anisonucleosis. C) Bcl-2. D) Neural cell adhesion molecule. E) Ki-67. F) SOX-10.
The patient stayed in hospital for a week, where their endopleural tube secretions, Hb, and haematocrit levels being closely monitored. After a day without endopleural secretions, the endopleural tube was removed. The day after that, the patient was discharged from the hospital after 21 days with no significant medications or further treatment adherence needed. They did not present any lack of tolerability after the surgical treatment. In the follow-up consultations, the patient had a full and successful recovery, a conclusion that was determined by assessing and comparing daily life activity limitations before and after the procedure, which had no significant change. There were no adverse or unanticipated events related to the treatment.
DISCUSSION
Schwannomas are benign, well encapsulated, slow growing, nerve intersecting fascicle tumours, which are composed exclusively of Schwann cells.3 They often present as a single tumour and are most commonly found in patients between 20–50 years old. They are found incidentally, since they do not present with any specific symptomatology.4
Around 90% of the schwannomas are sporadic, although they occur in specific syndromes like neurofibromatosis Type 2, schwannomatosis, and Carney complex.4,5 Some genetic studies have suggested that chromosome 22 plays an essential role in schwannoma development.
Schwannomas have a predilection for persons between the ages of 50–60. In addition, males are more commonly affected than females.6 Generally, these tumours are located in the head, neck, and flexor surfaces of the extremities. They are not often located in the mediastinum and retroperitoneum.
Pleural schwannomas are extremely rare neoplasms of the thoracic cavity,5 and less frequently in the pleura, with around 20 cases reported in the medical literature. Schwannomas grow slowly and, since they are generally asymptomatic, other differential diagnoses cannot be considered; however, larger tumours may compromise adjacent structures and cause cough, dyspnoea, and chest pain.7,8 Therefore, the vast majority of pleural schwannomas are discovered incidentally during investigations for other complaints.9
Unfortunately, plain radiographs are not specific enough, which is why MRI or CT scans can be used as diagnostic tools as well, to clarify the differential diagnosis between solitary pleural lesions, such as lipomas, liposarcomas, haemangiomas, elastofibromas, single metastatic lesions, mesotheliomas, fibrous tumours, and other neurogenic tumours.2,6
Histologic differential diagnosis includes spindle cell tumours, such as neurofibroma, leiomyoma, leiomyosarcoma, and calcifying aponeurotic fibroma. Antoni A and B areas are found microscopically in most cases of pleural schwannoma. Antoni A shows areas of hyper-cellularity with Verocay bodies. Antoni B represents areas of myxoid hypocellularity exhibiting degenerating changes such as cystic formation, calcification, haemorrhage, xanthomatous infiltration, and hyalinisation.9
The preferred treatment consists of surgical therapy, consisting in local resection of the tumor.10 Stereotactic radiosurgery is useful if the growing tumour is near vital blood vessels or nerves.11 In all schwannoma cases, an intraoperative frozen section should be carried out for histopathological examination and immunohistochemical staining in order to reach an accurate diagnosis.12 Prognosis is excellent and recurrence after resection is uncommon.
Schwannomas are rare; however, the authors have specifically discussed pleural schwannomas, which they say is an extremely rare disease, where there is not much literature available.
As seen above, the medical multidisciplinary team had all the necessary resources in order to provide an excellent diagnosis and treatment, which is not always the case when reporting a rare disease or case. Sharing the histopathologic features of schwannoma is not common and usually the available case reports lack images.
The patient was able to recover fully and had no significant or severe complications associated with medical care.








