Abstract
Objective: To determine the fetomaternal outcome of venous thromboembolism in pregnancy at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
Methods: This was a prospective cohort study of females with venous thromboembolism (VTE) in pregnancy at MTRH. These patients were followed up, and pregnancy outcomes were compared with a comparison arm of normal pregnant females (non-exposed). Purposive sampling was used for the non-exposed arm. Data were analysed using both descriptive and inferential statistics at 95% confidence level. Categorical variables were summarised as frequencies and percentages. Bivariate analysis was done using Chi square and multivariate analysis using logistic regression, with a confidence level of 95%. A p value of <0.05 was considered to be statistically significant.
Results: The mean age of the participants was 27 and mode of 22 years. Seventy percent of the study population were between the age of 18–35 years, with those below the age of 18 being one in both arms. Fifty-nine percent of females were multiparous. The most common site of deep vein thrombosis was superficial femoral vein, followed by popliteal vein (10 individuals; 5.3%). Multiparty was significantly associated with VTE (p=0.004). Females who were overweight or obese were associated with risk of VTE (p value of 0.001 and 0.003, respectively). There was a significant association between rates of Caesarean section and VTE (p=0.019). Postpartum haemorrhage, admission to newborn unit, and birth weight were associated with VTE with p value of 0.034, 0.025, and 0.018, respectively.
Conclusion: The authors concluded there is no difference in fetomaternal outcome between females with VTE and females without VTE.
![]()
Corrigendum: Fetomaternal Outcomes of Venous Thromboembolism in Pregnancy at Moi Teaching and Referral Hospital, Eldoret, Kenya
Authors: Dennis Odhiambo, Peter Itsura, Bett Kipchumba, Jack Odunga
Original citation: https://doi.org/10.33590/emjreprohealth/CJEB7192.
Date correction published: 19.08.24
In the article by Odhiambo et al., the N value for Apgar score in Table 1 has been updated to be ‘47’ as it was previously missing. In Table 2, the P values for 25.0–29.9 kg/m2 BMI, primiparous parity, no postpartum haemorrhage, no admission to neonatal unit (NBU), and birth weight of >2,500 g have been updated to be ‘1’ as they were previously missing. The definition of ‘Reference’ in both Table 1 and Table 2 has been added to the corresponding table legends, meaning ‘Baseline value for analysis’. This has now been corrected in all versions.
The authors apologise for any inconvenience caused.
![]()
Key Points
1. The findings of this study will be able to establish the gestation and mode of delivery that offers the best outcome for both mother and neonate, in females with venous thromboembolism (VTE) in pregnancy.
2. There is limited knowledge on how VTE affects the outcome of pregnancy in the African population. This study explains fetal and maternal outcomes of females diagnosed with VTE, by comparing their outcomes to females without VTE. This study also explains the risks of VTE in pregnancy.
3. The study found no difference in fetal and maternal outcomes between females with and without VTE. Those with VTE in pregnancy should be allowed to deliver at term, and attempt vaginal delivery, if there are no obstetric or medical contraindications.
INTRODUCTION
The development of a blood clot (thrombus) in a deep vein, usually in the lower limbs, is known as deep vein thrombosis (DVT). Pain, swelling, redness, warmth, and engorged superficial veins are examples of nonspecific symptoms.1 A potentially fatal condition known as a pulmonary embolism results from a clot breaking loose, and moving into the lungs. Venous thromboembolism (VTE) is the collective term for the illness process that results from DVT and PE.2
Pregnancy raises a woman’s risk of VTE by a factor of 2–4. According to research by Girish,3 there is a notable tendency for venous thrombi to develop in the left leg during pregnancy. This may be partly because the right iliac artery compresses the left iliac vein when they cross.3
Objectively confirmed DVT appears to occur with similar frequency in each of the three trimesters, despite the fact that leg swelling and calf pain are most common in the third trimester. Therefore, the vast majority of females with leg swelling, with or without calf pain, in the third trimester do not have DVT, whereas when left leg symptoms occur in early pregnancy, DVT is much more likely to be present.4
According to a 2009 study by Galanaud et al.,6 DVT in the lower extremities can be classified as proximal (thigh vein) or distal (calf vein).5 Since proximal vein thrombosis is more frequently linked to serious, chronic diseases, such as active cancer, congestive failure, respiratory insufficiency, and age greater than 75, it is more significant clinically than distal vein thrombosis, which is more frequently linked to transient risk factors, such as recent surgery, immobilisation, and travel.6
There is clear paucity of data on a number of key areas in the management of VTE in pregnancy. The time to deliver females with VTE in pregnancy and intrapartum management in cases of prolonged induction of labour is one of the major gaps. Very few studies have looked at the impact of VTE on the pregnancy, and how it affects pregnancy outcomes as compared to normal pregnancies.
This study seeks to bring forth a comparative analysis of fetomaternal outcomes between females with and without VTE in pregnancy.
Problem Statement
VTE, though rare, occurs more commonly during pregnancy and puerperium than in the normal population. At a rate of 0.5–2.2 per 1,000 pregnancies, it is a significant contributor to maternal morbidity and mortality, in both industrialised and developing nations, and accounts for 1.1 deaths per 100,000 pregnancies.7 Pulmonary thromboembolism, which is part of the VTE spectrum, has a high fatality rate. VTE is among the causes of near miss, with highest fatality rate of almost 100%; hence, prevention through early treatment of VTE is paramount.8
Pregnancies with VTE can either be allowed to go into spontaneous labour, or are induced at term to allow for continued care of the mother without any further compromise to the mother, especially in pulmonary thromboembolism. An area that is not clearly defined is the duration in which a female on treatment for thromboembolism can stay without anticoagulation during the period of labour, and induction of labour, bearing in mind that the risk of thrombus propagation is increased by the gravid uterus pressing on the pelvic vessels, causing stasis, which is part of the risk factors for VTE.9
A lot of studies have been done on the clinical presentation and patient risk factors for VTE in pregnancy and puerperium, but there is limited knowledge on how VTE affects the outcome of pregnancy in the African population, and locally in Kenya. The maternal outcomes of interest are gestation at delivery, Caesarean section, and postpartum haemorrhage. Fetal outcomes of interest are: preterm birth, 5-minute Apgar score, and admission to newborn unit (NBU).
Study Objective
To determine the fetomaternal outcome of VTE in pregnancy at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
METHODOLOGY
Study Site
The study was done in Eldoret, Kenya, at Moi Teaching and Referral Hospital (MTRH) in antenatal outpatient clinics, and maternity wards at Riley Mother and Baby Hospital, Eldoret, Kenya, in the gynaecologic ward, and the memorial private maternity wing of MTRH.
Study Design
This was a prospective cohort study. All pregnant females diagnosed with VTE were recruited at first point of contact, and followed up during the entire pregnancy until delivery. Females with no complications during pregnancy were matched with each case of VTE in the cohort arm. Every case was matched with three controls (i.e., 1:3). The 1:3 ratio was chosen to increase the power of statistics to detect a difference, and to make sure the results did not happen by chance. Matching was done based on parity and age with a margin of error of 5 years and 5 weeks being acceptable. Matching of cases was within 72 whours of case identification.
Sampling Technique
Consecutive sampling was used to recruit patients in the study.
Ethical Consideration
Approval was sought and obtained from the Institutional Research and Ethics Committee (IREC) at MTRH and Moi University School of Medicine, Eldoret, Kenya.
Data Collection
Questionnaires were administered for primary data collection, while patients’ files were used for secondary data collection. Secondary data gaps and inconsistencies were corrected through patient clarification at the time of data cleanup, which was done within 24 hours of attaining the information. For each questionnaire of a VTE case, the matched three subjects were interviewed, to allow for easy data analysis and comparison.
There was a pilot study conducted to test and retest the questionnaire before the main study started. This was done to standardise the data collection tools.
Primary data included bio-data, risk factors and clinical presentation, and pregnancy outcome (maternal and fetal).
Secondary data included how the diagnosis was confirmed, whether based on clinical symptoms or using radiological modalities.
Data Management and Analysis
Descriptive statistics for the measures of central tendency and dispersion, such as the mean and standard deviation, were used to summarise continuous variables, such as age, and Apgar score if normality assumptions will be satisfied. Categorical variables, such as admission to the NBU, preterm birth, or stillbirth were summarised using frequencies and the corresponding percentages. Continuous variables, such as age, gestational age, weight, and BMI, among others, will be summarised using mean and the corresponding standard deviation.
Maternal outcomes among females with VTE were summarised using the descriptive statistics for the measures of central tendency and dispersion. Frequencies and the corresponding percentages were used to summarise categorical variables, such as postpartum haemorrhage, and mode of delivery, among others.
Neonatal outcomes for females with VTE were summarised using descriptive statistics. Continuous variables, such as birth weight and Apgar score, among others, were summarised using mean and standard. Frequencies and the corresponding percentages were used to summarise categorical variables, such as admission to the NBU, preterm birth, or stillbirth, among others.
Fetomaternal outcomes were compared using appropriate statistical tools (STATA version 12 SE, Statacorp, College Station, Texas, USA). Preterm birth, stillbirth, and admission to NBU, among other categorical outcome variables, were compared between mothers with VTE and those without VTE, using Pearson’s Chi-squared test. Continuous variables, such as birth weight, Apgar score, gestational age, and quantity of blood lost, among other continuous variables, were compared between mothers with VTE and those without, using independent samples t test.
RESULTS
A total of 188 participants were recruited into the study. Of these, 141 were controls, while 47 were cases. Twenty-two of the cases had a previous history of VTE (Table 1).
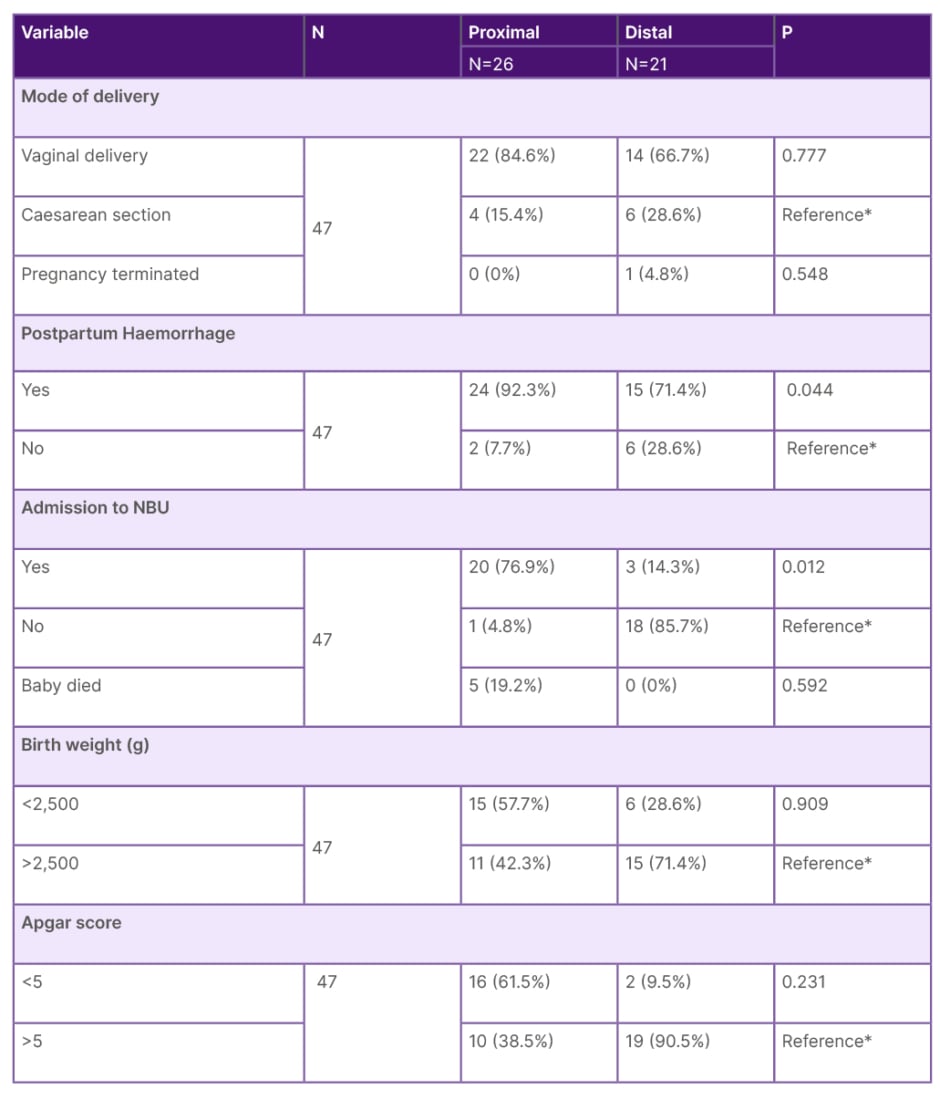
Table 1: Bivariate analysis between venous thromboembolism site and fetomaternal outcomes.
*Baseline value for analysis.
NBU: newborn unit
The majority of the population studies were between the age of 18–35 years in both cases, and control groups, with those below the age of 18 being one in both arms (assent given).The mean age of the participants was 27 years, with standard deviation of 6.13 years and mode of 22 years (8%). The majority of females studied (59%) were multiparous.
The superficial femoral vein (30%) was the most prevalent site of DVT, followed by the popliteal vein (10%), while 21% of patients had DVT in more than one location. Superficial femoral vein (30%) was most common site of VTE, while deep femoral vein (4%) was the least that occurred in isolation. Twenty-six cases (55%) had proximal VTE, whereas 45% had distal VTE.
Vaginal delivery was the commonest mode of delivery among cases with no statistical difference between proximal and distal VTE. Twenty-four of the cases with proximal VTE (92.3%) had a statistically significant association (p=0.044) with PPH as compared to distal VTE.
Females with proximal VTE had more admission to NBU compared to distal VTE (76.9% and 14.3%, respectively), which was statistically significant (p=0.012) The rest of the outcomes were not statistically significant.
Five percent of cases (24/47) where diagnosed at third trimester, with the lowest number in first trimester (6/47). There was an association between parity and VTE. It clearly came out that multiparity is significantly associated with VTE (p=0.004).
There was no statistically significant difference in the gestational age at delivery for both cases and controls, as most deliveries were term seven (1.6% and 80.9% for controls and cases respectively).
The majority of the population delivered vaginally (148/188). Only one pregnancy was terminated amongst the participants, due to fear of warfarin embryopathy because she conceived while on long term warfarin anticoagulation. The majority of cases had vaginal births (37/47; 78%).
There was a significant association between rates of Caesarean section and VTE (p=0.019.) There was also a statistically significant association between postpartum haemorrhage and VTE (p=0.034). Admission to NBU and birth weight were also associated with VTE (p value of 0.025 and 0.018, respectively); however, the study found no association between blood group and VTE.
Multivariate analysis showed that the participants with a BMI of more than 30 had a four-times higher risk of having negative outcomes than those with a BMI of 17–25 (Table 2). The results also had a statistically significant P value of 0.001. Similarly, multiparous females were also two-times more likely to have negative outcomes than primiparous, with a significant P value of 0.032.
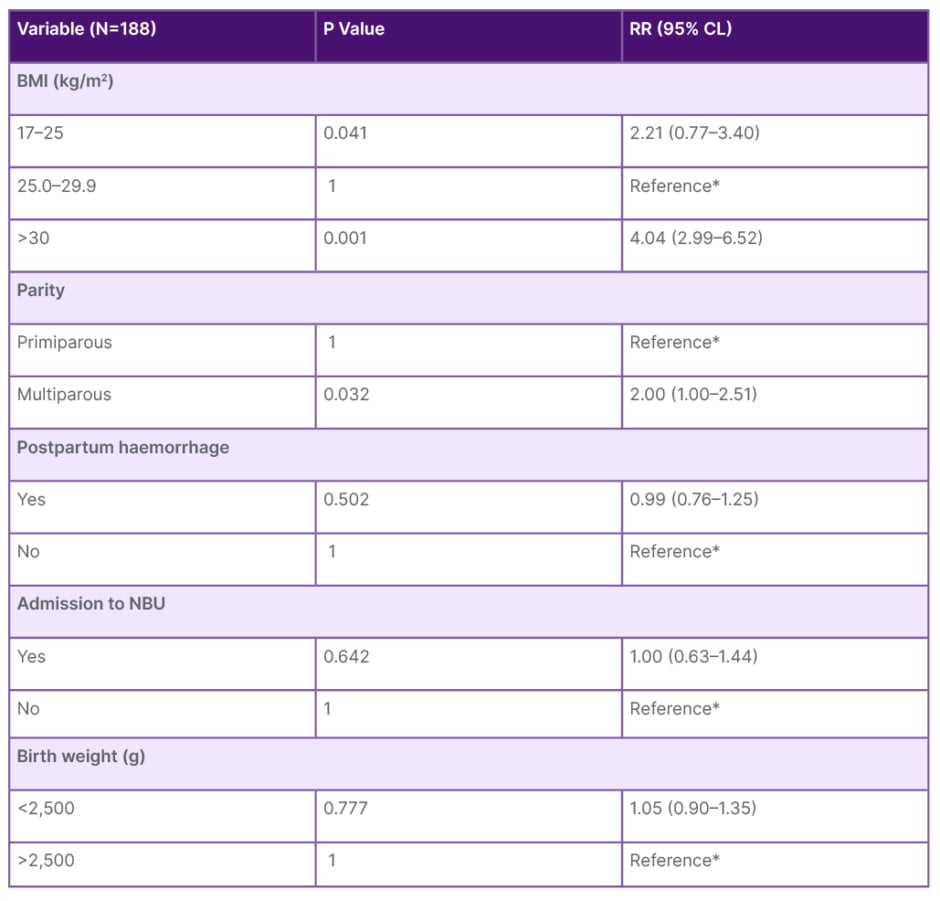
Table 2: Multivariate logistic regression after adjusting for confounding variables.
*Baseline value for analysis.
CL: confidence limits; NBU: newborn unit; RR: relative risk.
DISCUSSION
Obesity and Venous Thromboembolism in Females
In this study, obesity with BMI >30 was found to be a strong independent risk factor for VTE (AOR 4.94). This was in agreement with available data that implicate obesity as an even stronger risk factor for VTE than for coronary heart disease and stroke.4 Previous publications from the Hoorn Study showed that obesity is a risk factor for VTE.10
The mechanisms of how obesity increases the risk of VTE was correlated with increased thrombin generation and peripheral conversion of androstenedione to oestrogen in adipocytes (fat cells), particularly in females with obesity.10
Parity and Risk of Venous Thromboembolism
In this study, multiparity was found to be an independent risk factor for VTE (adjusted odds ratio [AOR]: 2.22). This was in agreement with studies by Jacobsen et al.,13 and Zotz et al.,18 that found multiparity increased the risk of VTE in pregnancy; a study by Waldman et al. also confirmed that multiparity, especially grand multiparity, increases the risk of VTE.12
Gestation Age at Diagnosis
In this study, the gestational age at diagnosis was mainly in the third trimester (51%). These results are in agreement with not only a study done in Nigeria, where majority of the cases were diagnosed during the third trimester, but also another case control study in a referral hospital in Ghana.4,14
Maternal Outcomes
Gestation at delivery
In this study, the majority of the females in both arms delivered at term, and there was no statistically significant association between gestational age at delivery and risk of VTE. These results are supported by Ben-Joseph,15 who found no significant association between gestational age at delivery and VTE. However, several studies have associated gestational age at delivery and VTE risk. Zoller16 found a significant association between gestational age at delivery and VTE, with incidence of venous thromboembolic events being fourfold. Similarly, Galambosi17 also found that the risk of VTE was three-times higher in the females who delivered preterm compared with the females who delivered at term.
Mode of delivery
In this study 19% (nine) of cases compared to 21.39% (30) of controls delivered via Caesaerean section, which was not statistically significant. This was in agreement with studies by Zotz and colleagues,18 who found no relation between mode of delivery and VTE. These findings, however, differ from studies done by Dresang et al.19 whose findings were similar to those of Chang et al.,20 that showed a significant association between VTE and Caesarean section.
Onset of labour
For females on therapeutic anticoagulation, a planned delivery, either through the induction of labour, or by elective Caesarean section, may allow optimal timing of events, or minimise the risks of an unplanned delivery on full anticoagulation. Chan et al.21 found peripartum bleeding risk for females on therapeutic anticoagulation acceptable.
Postpartum haemorrhage
In this study, PPH was statistically significant at bivariate level, but no association after adjusting for confounders (AOR: 1.11) at multivariate analysis. This was in agreement with Chan,21 who found postpartum bleeding risk for females on therapeutic anticoagulation as acceptable.
In addition, a study by Kominiarek,22 on effect of low molecular weight heparin in pregnancy, showed that bleeding complications, including PPH and transfusion, were not increased when compared to normal controls matched for delivery route.
On the contrary, in a study done by James et al.,23 females with VTE are at an increased risk of postpartum haemorrhage during birth and childbirth.
A cohort study done by Chauleur et al.24 found out there is a risk of PPH during delivery; hence, they studied the relationship between severe PPH and VTE in females during their first pregnancy. Out of the 615 females with VTE recruited, 317 had postpartum haemorrhage, which was statistically significant (p=0.002).24
Fetal Outcomes
Birth weight
In this study, there was a significant association between low birth weight and VTE (p=0.018). A case control study done by Blondon et al.25 had the same insight, and beyond their study found out that delivery of a newborn with low birth weight is associated with a threefold increased risk of maternal postpartum VTE. Their conclusion was that this should be considered when assessing VTE risk at delivery, and during antenatal clinic visits.24 Another study by Tsai26 also had similar results, only in this case, the risk of VTE also affected the newborn, with newborns having a risk of developing VTE either in childhood, teenage years, or adulthood.26 Another study by Chaireti and Bremme27 also came up with the conclusion that there is a significant association between VTE and birth weight. In their study, it was ascertained that there is an association between birth weight and VTE,27 especially in females with antiphospholipid syndrome.
Apgar score at 5 minutes
This study did not find any association between Apgar score and VTE. Apgar score at 5 minutes of both arms was not different between the two groups, as they all had good Apgar score (p=0.433). This is supported by a case control study by Tuckuviene et al.,28 whose study had concluded that other independent infant, obstetrical, and maternal characteristics could be associated with low Apgar score, which may be associated with VTE and Apgar score outcomes.28
Admission to newborn unit
The authors’ study found a significant association between NBU admission and VTE (p=0.025). These results contradict the findings of Tuckuviene et al.,28 whose study found no significant association between admission to the NBU and VTE.28 The above findings could be attributed to the high number of preterm births and low birth weights in this cohort study.
CONCLUSIONS
Females with obesity and higher parity have a higher probability (AOR: 4.94 and 2.22, respectively) of getting VTE than the normal population. However, females with VTE were not at an increased risk of postpartum haemorrhage than those who did not have. There was no difference in gestational age at delivery between the cases and controls. There was no difference in the 5-minute Apgar score and NBU admission among the cases of VTE and controls. Low birth weight was more common among cases of VTE than controls.
The authors recommend larger longitudinal studies that will include the community, and for the major findings to be generalised for both the hospital setting and at the community level.
Strength and Limitations
The strength of this study was in the methodology. The study was powered enough to make sure that the results did not happen by chance. The limitation was that this was a hospital-based study, and the findings may not be the same with a community-based study.







