Interviewees: Nick Raine-Fenning,1 Michaël Grynberg,2 Stephen Hussey3
- Faculty of Medicine & Health Sciences, University of Nottingham, Nottingham, UK
- University Hospital Antoine Béclère, Clamart, France
- General Manager Women’s Health Ultrasound Europe & RCIS, GE Healthcare, Amersham Place, UK
Disclosure: Dr Nick Raine-Fenning is a shareholder at Nurture Fertility and an advisor to GE Healthcare, Merck, Ferring Pharmaceuticals, and Pharmasure. Prof Michaël Grynberg has received fees from Merck Serono, Ferring, Gedeon Richter, GE Healthcare, Samsung, and Cook Medical.
Support: The publication of this feature interview was supported and reviewed by GE Healthcare.
Acknowledgements: Medical writing assistance was provided by James Coker, European Medical Journal, London, UK.
Dislcaimer: The opinions expressed in this article belong solely to the named interviewees.
Citation: EMJ Repro Health. 2019;5[1]:26-33. DOI/10.33590/emjreprohealth/10312082. https://doi.org/10.33590/emjreprohealth/10312082.
Ultrasound (US) has been a frequently-used tool in the field of reproductive health since the mid-1950s. It has been hugely successful, especially during pregnancy, in helping to detect issues such as fetal abnormalities. It is also a non-invasive procedure, working by bouncing ultrasonic soundwaves at body structures or tissues and detecting the echoes that bounce back. The quality of US scans has continually improved over the years, and with emergent technologies, such as Doppler and three dimensional (3D) imaging, the ability for physicians to use US to accurately visualise organs and structures within the female pelvis is extensive. However, across the broad spectrum of reproductive health physicians, there appears to be significantly more scope for US to be utilised in daily clinical practice, particularly in treating infertility and increasing the success rates of procedures such as in vitro fertilisation (IVF).
To better understand the extent to which US can be utilised, the European Medical Journal recently interviewed two leading figures in reproductive health who are particularly strong proponents of a broad use of US in clinical practice. These were Dr Nicholas Raine-Fenning, Clinical Associate Professor & Reader in Reproductive Medicine and Surgery, Faculty of Medicine & Health Sciences, University of Nottingham, Nottingham, UK, and Prof Michaël Grynberg, Head of the Department of Reproductive Medicine and Fertility Preservation at the University Hospital Antoine-Béclère, Clamart, France. As well as providing a general overview of US across reproductive health, each provided an analysis from the perspective of their main area of clinical expertise: Dr Raine-Fenning focussed primarily on the use of US in IVF, while Prof Grynberg gave insights on its role in diagnosing infertility. In addition, Mr Stephen Hussey, General Manager, Women’s Health Ultrasound, Europe & RCIS, GE Healthcare, Amersham Place, UK, was invited to share a commercial perspective on the use of US technology in reproductive medicine.
INTRODUCTION
The importance of ultrasound (US) technology to the working practices of reproductive health physicians is difficult to overstate. “It is not so much a benefit, more an absolute necessity,” explained Dr Nicholas Raine-Fenning. “You could not practice reproductive medicine without US, it is a central part of everything we do every day: all patients have a scan as part of their fertility investigation to see if there is an underlying issue, as looking for pelvic pathologies, such as cysts, fibroids, polyps, uterine abnormalities, swollen tubes, or polycystic ovaries is crucial.”
“It is not so much a benefit, more an absolute necessity. You could not practice reproductive medicine without US.”
Prof Michaël Grynberg strongly concurred with this assessment, appreciating the critical role that US has to play throughout the whole cycle of assessment and treatment that an infertile patient will typically undertake, stating: “It is probably one of the main ways a fertility expert can profile the assessment of female infertility. It is certainly important for us in helping diagnosis because it can directly locate the aetiology of the infertility.” He added: “It is also important for planning the treatment strategy according to ovarian function because, from the results, we will be able to tell if a patient should be able to respond to the proposed fertility treatment which is primarily based around ovarian stimulation. It is important to measure and assess the ovarian response to our treatment.”
Considering the technological advancements in US that have taken place in recent years, there is a great opportunity to enhance patient care in reproductive health, while at the same time improving efficiency and reducing costs if US is used more widely. Mr Stephen Hussey added: “There has been a great deal of investment in US technologies that, when combined with the correct training, can help improve diagnostic confidence and at the same time provide more patient comfort during examination.” For instance, although there are no differences in patient preference for either procedure, hysterosalpingo contrast sonography (HyCoSy) is associated with less pain1,2 and is better tolerated when compared with using hysterosalpingography (HSG) to assess tubal patency.3
Despite this, the use of US is not as widespread as it could, or arguably should, be across this area of medicine. “If someone is seen in a general gynaecology or fertility clinic, they do not all get a scan,” explained Dr Raine-Fenning. “Unless they have got an indication for a scan, such as pain, heavy bleeding, etc., they tend not to be scanned. Rather, they tend to just get a vaginal examination, which has less sensitivity and specificity. I think all reproductive medicine professionals specialising in in vitro fertilisation (IVF) realise this and so tend to do scans at a lower threshold than in general gynaecology. In general gynaecology, US is often used as a baseline scan to exclude pathology in women with signs and symptoms; it is not used much after that. In IVF, it has a much more functional role.”
ULTRASOUND IN CLINICAL PRACTICE
Dr Raine-Fenning’s practice is primarily focussed on IVF, an area of reproductive health in which US underpins all aspects of treatment. Dr Raine-Fenning detailed how this plays a fundamental role in his day-to-day clinical work: “Before a patient even comes into the IVF unit, we scan them; that means when I first see them for their initial consultation, I can talk to them about any pathology that we have seen and whether they need surgery. Then when they start treatment, it is monitored by daily US scan, which tells us how they are responding and whether changes need to be made to maximise response and therefore outcome.”
It is this ability to accurately measure responses to treatment that Dr Raine-Fenning believes has had the most profound impact on the chances of a successful IVF treatment. “It has completely changed our practice, as we are able to dose more accurately and confidently,” he confirmed. “Ensuring they are on the right dosage of drugs from Day 1 reduces under and over-response. And that has revolutionised everything for us because, previously, we gave drugs to people based on their age and follicle-stimulating hormone level, which is a far inferior way to predict response.”
At the Department of Reproductive Medicine, Hôpital Antoine Béclère, Prof Grynberg and his colleagues have likewise ensured that US is used to the fullest extent throughout the team, ensuring that everyone they work with, from gynaecologists to midwives, are trained to perform thorough US scans on patients which provide reliable results. He informed us that, as a result of this emphasis, there are between 80 and 100 US scans that take place in the hospital each day. The focus of US in this context is on helping the varying needs of patients with fertility problems. “We perform US to diagnose infertility and, in those fortunate to conceive, to check for pregnancy, but we also offer US to those patients thinking ahead who want to preserve their fertility,” outlined Prof Grynberg.
“US is very helpful in enabling the physician to guide the patient to the best way of reaching the goal of fertility as quickly and as effectively as possible.”
In a similar fashion to the influence US has in Dr Raine-Fenning’s team, at Prof Grynberg’s department the results of an US scan will ultimately be the biggest factor in the type of treatment that is decided upon in a given case. “The decision in the end will be taken according to the patient’s age, sperm results, tubal patency, and ovarian function. Both tube patency and ovarian function will be assessed by US scan,” he elucidated. “For example, if you have a patient with a large number of eggs who is quite young, intrauterine insemination will be discussed as an option. And, for another young patient who has a low number of eggs and a low follicle count, they may be a direct candidate for IVF. So, US is very helpful in enabling the physician to guide the patient to the best way of reaching the goal of fertility as quickly and as effectively as possible.”
It is US’s ability to assess tubal patency that provides a pertinent example of how it can improve upon the kind of procedures that would otherwise be used. “Through using US we are able to assess tubal patency because we can use the US to monitor the flow of contrast media injected through the cervix,” said Prof Grynberg. The greater levels of safety and comfort patients have when US is used in this way compared with HSG examinations will be analysed later in this article.
Prof Grynberg then spoke about how US scans, which have improved in quality over the years, have been a major driver of improved outcomes at his clinical practice over the last 30 years. “We know we are more efficient in the diagnosis of infertility by better understanding the aetiology. And this leads to an overall improvement because it guides the physician in finding the best technique to offer to the patient, and probably provides the best method of measuring the efficiency of our treatments,” he outlined. “This is the result of many changes in the laboratory, for sure, but it is also due to US enabling physicians to be more precise in deciding treatments for infertility and the monitoring of those treatments.”
TECHNOLOGICAL ADVANCEMENTS
As previously alluded to, advancements in US technology are increasing the benefits these machines offer to reproductive health physicians. In Dr Raine-Fenning’s view, the most important aspect, above all others, is ensuring image and resolution is clear and of the highest possible quality: “Some US machines are quite poor. When you scan on a machine that has got less power driving it, it is so much harder. So, it is not just the availability of US, it is also the quality: it makes a massive difference.”
Likewise, Prof Grynberg sees machine quality as vital; making careful selection on the US scan being used should therefore be taken heavily into consideration by physicians. He stated: “I think the US machine is extremely important because, depending on the type of machine, you are able to see things that you would not see in others. So, with high quality machines, operator dependence will be much lower. The quality of the machine makes all the difference.”
Automated Measurements
Dr Raine-Fenning and Prof Grynberg also see the potential benefits that new technological features provide to specific aspects of the role US can play. One of these, automated measurements, has had a substantial impact for both of these experts, greatly enhancing their ability to count follicles. Dr Raine-Fenning said: “When it works, it is very good. Even though it is not exactly spot on in terms of accuracy, it is very good for reliability, because the beauty of automated US is that it does not count follicles twice; this really improves your ability to count. So, for an objective measure of the numbers, it is brilliant, but we still need to work on measurement of size and volume.” Dr Raine-Fenning emphasised that good image quality is vital for this to occur.
Having an automatic measuring capability is also vital for the day-to-day work of Prof Grynberg. Again, machine quality is the defining factor in ensuring this capability works well. “We have a Voluson™ E8 [GE Healthcare, Illinois, USA] machine, which is one of the best for assessing infertility because we are able to get a very good picture of the ovaries, which allows us to have an automatic follicle count,” he explained. “This follicle count is a key issue for us, both in planning for and follow-up of treatment.”
Mr Hussey is similarly acutely aware of the impact this feature can have for physicians.4 “Automated assessment tools, designed in collaboration with leading reproductive medicine specialists, can help enhance accuracy, improve independent user reproducibility, and shorten exam times. Such technologies are becoming increasingly important to help enhance the potential diagnosis, screening, and treatment success,” he noted.
Three-Dimensional Technology
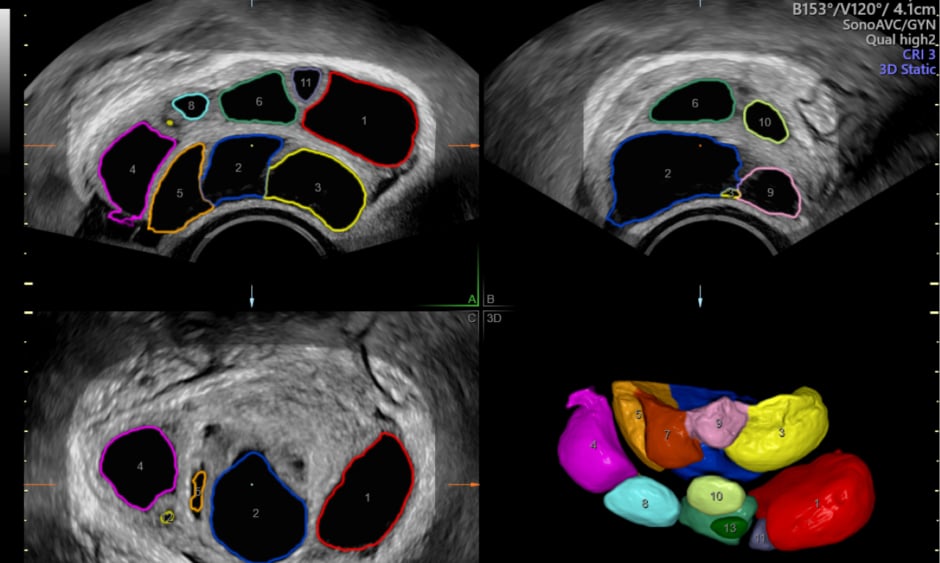
Another prominent feature that can be included with US machines is 3D technology, which provides more detail and images not possible with 2D. This has become a necessity for analysing the uterus, especially regarding the discovery and classification of uterine abnormalities. Prof Grynberg outlined how areas such as the uterine cavity cannot be viewed as extensively using a traditional 2D US. He went on to describe the ways in which 3D technology can be used to improve the reliability of automatic follicle counting, citing how the SonoAVC™ (GE Healthcare, Illinois, USA) follicle automatic counting model has substantially enhanced the measuring of ovarian follicles at his department: “When you do it with the 2D, we know we probably miss some of these follicles because it is not possible to make sure we are assessing the whole ovary. But with 3D we can observe the whole ovary even while moving the probe from one place to another. And by using automatic counting with the SonoAVC, we know that with a 3D view all the fluid structures can be counted with reliability.”
Dr Raine-Fenning is also a proponent of 3D being used in this manner; however, he believes that there is limited recognition of this among reproductive health physicians. “It is the gold standard and the only way to diagnose uterine abnormalities with confidence,” he commented. “It helps with everything; if you are doing a measurement, then the spatial orientation is much better with 3D compared with 2D. It is not used in that way by most people; most use it for uterine abnormalities alone, but it is also a great way of viewing data and measuring as you have three reference points.”
Mr Hussey also shared his experience of the benefits that a 3D view can provide to physicians: “3D US of the pelvis can be used routinely to diagnose uterine abnormalities as it enables unprecedented views of the uterus and endometrium in a coronal plane.”5
ENHANCING THE PATIENT EXPERIENCE
US scans in reproductive health are not just highly beneficial to clinicians; they can substantially improve the experience of patients in a clinic. There are several reasons for this. One is by reducing the need for invasive procedures such as manual vaginal examinations; another is that the more detailed information a physician can collect from US scans can allow them to better guide and explain to patients what their treatment options are, enhancing patient knowledge and thereby the role they can play in their own care.
To emphasise this point, and from his own personal experience, Dr Raine-Fenning has used US to correct misdiagnoses on a number of occasions: “We have lots of people who come from clinics and been told they might have a uterine abnormality but it is often unclear. We rarely have such disparity; we scan in 3D and can confidently tell a patient what their pathology is.
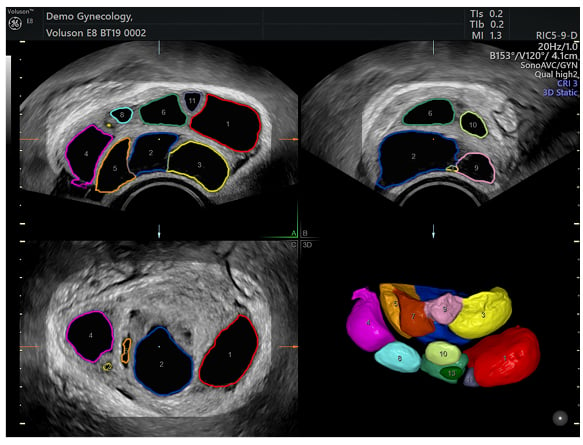
Figure 1: Example of a volume acquisition of the ovary using SonoAVC Follicle ™ – 3D volume technique that automatically counts and measures follicles.
Uterine anomalies can be diagnosed with 100% concordance and we can also subclassify the type removing any confusion. Patients appreciate this and leave with renewed confidence and complete understanding.”
As alluded to earlier, analysing tubal patency is one area where using US can be far more beneficial to patients than a HSG X-ray examination. One reason for this is that it is much safer. “US techniques such as HyCoSy or hysterosalpingo-foam sonography, for example, can offer information on tubal patency without the harmful effects of radiation exposure necessary in HSG examinations,” said Mr Hussey. Women undergoing HSG are exposed to pelvic radiation. The mean dose-area product (DAP) for a complete HSG examination is 2.05 Gy cm2. In comparison, the mean DAP for a single posterior–anterior chest X-ray examination is 0.09 Gy cm2.6 In contrast, there is no exposure to radiation associated with HyCoSy and CAT.
As well as mitigating the need for radiation to be present, using US for the purpose of determining tubal patency can be a far less invasive, more comfortable, and less time-consuming process for the patient in comparison to HSG. “The HSG exam is difficult for the patient because it can be painful, so by using US and combining the administering of the foam gel, the procedure is definitely less invasive for the patient,” commented Dr Grynberg. “In addition, it does not require any radiation exposure; these are all benefits for the patients and the physicians too because it allows us to have what we call a fertility 1-day check, where we assess the ovary, uterine cavity, and tube.”
AWARENESS AND TRAINING
Despite the fact US can make such a profound impact on the work of clinicians, and indeed on the lives of patients, it is apparent that, particularly in certain areas of reproductive medicine, it is not used to its full capacity, partly due to lack of awareness and partly due to lack of training. Dr Raine-Fenning outlined: “The training of obstetricians is engrained in US; every assessment they do is in US. But in gynaecology, for example, US does not seem to form a key part of training, so I think generally in gynaecology, the level of knowledge of US and its application is a lot poorer because there are so many people who are not brought up with scanning.”
Drawing on his own experience of organising and teaching a 3D US scanning course, Dr Raine-Fenning has observed just how much room there is for the improvement of reproductive health specialists in terms of knowledge and skill in using US. “I have had doctors from all over the world come on my 3D course and they have all got potential to keep on learning,” he commented. “Within a few hours I realise the standard level is quite low, and not just 3D US but basic 2D US as well. I think the machines are ahead of many of the users so training and standardisation in US is what is needed now. We simply must make the most of what we already have.”
“We need to make sure that everybody is aware that US is probably the most important tool for the fertility worker.”
Ensuring that the understanding of the full potential of US, as well as extensive training in its use, is part of the curriculum of medical students in the reproductive health field should therefore be a high priority. As a renowned university hospital, at the Hôpital Antoine-Béclère a major emphasis is placed by Prof Grynberg and his team on ensuring that all junior doctors learn the processes and skills they need to be proficient in using US. More generally, Prof Grynberg argues that a more thorough US training programme needs to take place at an early stage of a physician’s development. “US is now a big aspect of the training of young medical students, particularly those who want to specialise in obstetrics. So, they know how to perform an overall US, but for those who want to go further in reproductive medicine, we need to train them more and this can be performed in universities.

Figure 2: An image of the uterus demonstrating the endometrium in the coronal plane, acquired in 3D volume acquisition mode.
We need to make sure that everybody is aware that US is probably the most important tool for the fertility worker,” he said.
Dr Raine-Fenning, with his vast experience in training others on US, noted that the key to becoming proficient in US scanning is constant practise. While online videos and simulation are helpful, nothing can replace hands-on experience in his view. That is his advice to physicians in this area: repetition. “I have always said the key to US is to be able to recognise normality, if you know it is not normal, then you can refer to the relevant person if necessary. The more you do it the quicker you will start recognising normality and therefore abnormalities: it is all about pattern recognition,” he said.
CONCLUSION
While US has been a staple in reproductive health for several decades, advancements in machine quality and the advent of features such as 3D and automated measurements have enhanced the potential it has to be used across virtually all stages of a patient’s cycle during pregnancy or when seeking fertility treatment. In the examples shared in this article, US has revolutionised the clinical work of Dr Raine-Fenning and Prof Grynberg in making diagnoses, discovering underlying pathologies, and predicting and assessing the impact of treatment. Increasing use of US in this area of medicine can not only improve patient outcomes but patient experiences too, with US being more accessible and far less invasive than alternative imaging methods. A greater emphasis on explaining its importance, as well as providing more opportunities for practical training of physicians in all areas of reproductive health, is clearly a major requirement moving forward.
Biographies
Dr Nicholas Raine-Fenning Faculty of Medicine & Health Sciences, University of Nottingham; Clinical/Scientific Director, Nurture Fertility, The Fertility Partnership, Nottingham, UK
Dr Raine-Fenning is an internationally recognised expert in three-dimensional ultrasound and gynaecological imaging, regularly providing lectures and leading plenary sessions and workshops in this area. Among a host of prominent positions, he is a board member and Vice Chair of the Scientific Committee of the International Society for Ultrasound in Obstetrics & Gynaecology (ISUOG). In his clinical role, Dr Raine-Fenning manages women with benign gynaecological pathology and subfertility undergoing IVF treatment.
Prof Michaël Grynberg Department of Reproductive Medicine and Fertility Preservation, University Hôpital Antoine-Béclère, Clamart, France
Prof Grynberg is considered a pioneer on the topic of female fertility preservation, having undertaken numerous research projects in this area. Other research interests include assessment of ovarian follicular status and the regulation of anti-Müllerian hormone (AMH). His clinical work is based around the diagnosis and treatment of subfertile or infertile couples.
Mr Stephen Hussey General Manager Women’s Health Ultrasound Europe & RCIS, GE Healthcare, Amersham Place, UK
Mr Hussey has over 20 years’ experience working in medical ultrasound sales, having started his career as a clinical applications specialist before progressing into sales and commercial product management. Previously, Mr Hussey trained as a radiographer and sonographer, gaining invaluable experience in obstetrics and gynaecology while working at both Hereford County Hospital and the Birmingham Women’s Hospital.