BACKGROUND
Current management of recurrent pleural effusion is symptomatic. Indwelling pleural catheters (IPC) reduce the initial length of hospital stay1,2 but require repeated domiciliary drainage. Talc pleurodesis is a potential one-time definitive procedure but has a modest failure rate. In cases of talc pleurodesis failure, IPC insertion is usually advocated with the consequence that a subset of patients with IPC in situ will have previously received ipsilateral intrapleural talc.
Non-draining symptomatic septated IPC-related pleural effusions (NSSIPE) complicate up to 14% of IPC insertions, and may require further procedures, including those aimed at disrupting septations.3-6 Given the larger pleural tumour bulk and greater area of pleural involvement with mesothelioma than with other malignant pleural effusions (MPE),7 mesothelioma may be associated with increased risk of fibrin deposition and septation formation.
This study aimed to assess whether prior failed talc pleurodesis is associated with increased risk of NSSIPE.
METHOD
IPC insertion records from January 2008–April 2017 were analysed retrospectively. Standard management in our unit during this time was to offer patients with recurrent pleural effusion a choice between chest drain insertion with talc pleurodesis or IPC insertion.
NSSIPE was defined as a symptomatic pleural fluid collection with septations evident on pleural ultrasound in the context of a non-draining patent IPC.
RESULTS
There were 202 recorded IPC insertions. The non-MPE group included 21 patients with a mean age of 70 years (standard deviation [SD]: 10.8 years) and 29% (n=6) were female. In this group, the underlying causes were attributed to hepatic hydrothorax (3% overall), benign pleuritis (3%), heart failure (2%), and others (2.5%). The MPE group consisted of 181 patients with a mean age of 68 years (SD: 13.9 years; p=0.4) and 48% were female (n=87; p=0.09).
There was no statistically significant difference between rates of NSSIPE in patients who had received prior talc and those who had not, as well as between patients with mesothelioma MPE and those with non-mesothelioma MPE (Figure 1).
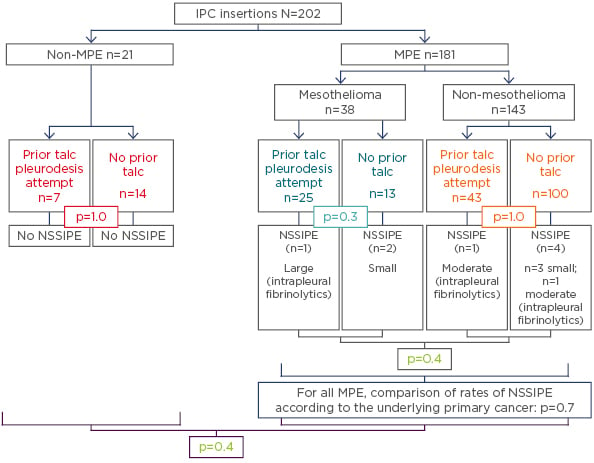
Figure 1: Rates of non-draining symptomatic septated indwelling pleural catheter-related pleural effusions in patients who had received prior talc and those who had not, as well as rates in patients with mesothelioma malignant pleural effusion and those with non-mesothelioma malignant pleural effusion.
IPC: indwelling pleural catheters; MPE: malignant pleural effusion; NSSIPE: non-draining symptomatic septated IPC-related pleural effusions.
DISCUSSION
Non-draining MPE are associated with a higher concentration of pleural fluid lactate dehydrogenase and systemic C-reactive protein, indicating an association between increased pleural fluid metabolic activity and systemic inflammation.4,5,8 The aim of giving talc is to induce an inflammatory response within the pleural space, leading to adhesion formation between the visceral and parietal pleura, with subsequent pleurodesis.
The results of this study raise interesting questions. For example, in cases of failed talc pleurodesis, why is it that talc is not associated with increased rates of NSSIPE? It may be that if a patient is unable to mount an adequate immune response to talc, and, therefore, has failed talc pleurodesis, then the patient is also unable to mount an adequate immune reaction to talc to form adhesions and septations within the pleural space.
These results are limited by the retrospective study design and the relatively small number of NSSIPE. Further analyses will investigate whether the stage of tumour at which talc was given influenced rates of NSSIPE, and further studies are required to investigate whether the pleural space in certain patients is inherently resistant to different forms of pleurodesis.
CONCLUSION
Talc pleurodesis remains an important alternative to IPC insertion in recurrent pleural effusion. The risk of NSSIPE is not increased in patients with a prior talc pleurodesis attempt. Therefore, the risk of subsequent NSSIPE should not dissuade patients from choosing talc as a primary treatment for recurrent pleural effusion.








