BACKGROUND AND AIM
Pneumomediastinum (PM) is a rare pathological entity that is divided into two categories: secondary, with a well-known aetiology, and spontaneous, with no clear aetiological factor.1 At the beginning of the COVID-19 pandemic, some publications demonstrated PM as a complication of COVID-19 pneumonia.2-4 In the authors’ thoracic surgery practice, they established incidences of PM in patients with COVID-19 pneumonitis. Therefore, they decided to highlight the importance of PM with its two types, secondary and spontaneous, in COVID-19 pneumonia.
RESULTS
The authors’ present three patients with COVID-19 pneumonia and pneumomediastinum. A 78-year-old woman with PM diagnosed on Day 12 of mechanical ventilation. The day after establishing PM, a control chest X-ray demonstrated shifting of the mediastinal structures to the right hemithorax, with apical left-sided pneumothorax. A left-sided chest tube drain was inserted. The woman’s respiratory status was progressively worsening, and she died of multiple organ dysfunction syndrome on Day 23 of intubation.
The other two patients were 58-year-old and 75-year-old men with PM as a late consequence of COVID-19 pneumonia (on Day 47 and Day 28, respectively, after diagnosis of COVID-19 infection).
They were admitted with clinical symptoms of a dry cough, shortness of breath, chest pain, and subcutaneous neck emphysema and PM was determined by a thoracic CT. After 10 days of conservative treatment, the 75-year-old man was discharged in a good condition, with a significant reduction of PM. On the second day of hospitalisation, the 58-year-old man expressed severe dyspnoea and progression of subcutaneous emphysema to the chest, neck, face, and arms. A control chest CT determined progression of PM with left-sided apical pneumothorax (Figure 1). A chest tube drain was inserted. The patient’s respiratory status continued to worsen with exitus on the second day after chest drain insertion.
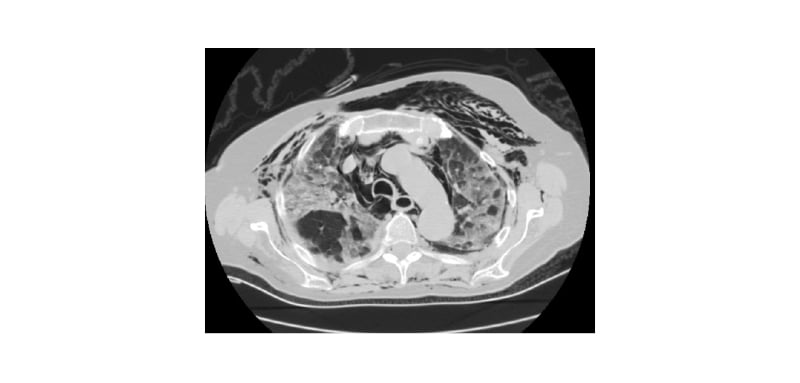
Figure 1: Chest CT of bilateral lung patchy ground-glass opacities, pneumomediastinum, left-sided pneumothorax, and significant expressed subcutaneous emphysema.
CONCLUSION
The authors accepted the destructive viral effect on the alveoli as the main predisposing factor for spontaneous type of PM in COVID-19 pneumonia. In cases with mechanical ventilation with positive airway pressure support, the authors consider barotrauma as an aetiological factor on secondary type of PM.
They concluded that a concomitant spontaneous pneumothorax was ‘secondary’ as a result of alveolar rupture, due to the viral-induced pneumonitis and/or positive pressure ventilation.
With this study, the authors highlight the PM in its two forms (secondary and spontaneous) to be a serious COVID-19 pneumonia complication, even in the post-COVID-19 period. Their study points out to be alert of PM in COVID-19 pneumonia, even in the patients with no need for mechanical ventilation.








