Milan, Italy, a city renowned for its style and beauty, provided a splendid setting for the 27th ERS International Congress. As the attendees discovered, Milan is about much more than just fashion, with magnificent architecture, such as the Milan cathedral, a vibrant opera scene, including the Scala Opera house, and a tradition and history to rival cities worldwide.
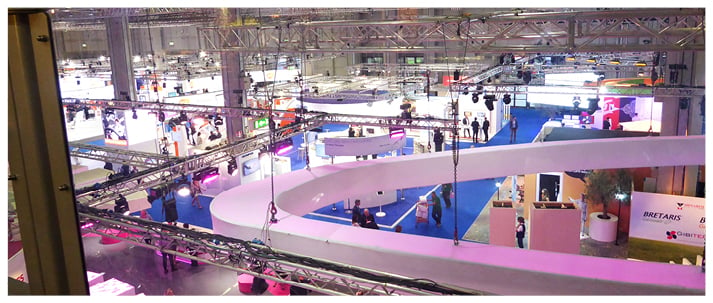
A highly entertaining opening ceremony began with some typically beautiful Italian opera signing, including a rendition of the world famous ‘La donna e mobile’ by Luciano Pavarotti. This was followed by a wonderfully crafted video that showed the congress Chair Prof Francesco Blasi, and Co-Chair Prof Stefano Centanni in various scenic locations in Milan, with Prof Blasi appearing to sing the famous Pavarotti piece ‘Nessun Dorma’ and Prof Centanni driving an Alfa Romeo car! This last homage was particularly fitting, as the location of this event, the MiCo congress centre, was formerly the factory of Alfa Romeo.
During his address at the ceremony, Prof Blasi expressed his excitement that the largest respiratory event in the world was returning to Italy for the first time in 17 years. He also gave a final figure on the number of participants for this year’s congress, totalling a whopping 21,080. ERS President Prof Guy Joos was also on hand to inform the captivated audience about some of the aims, work, and campaigns of the society. “We have the mission to promote lung health in order to help our patients and to drive the standards for respiratory medicine. To do so we are concentrating on three different pillars: the activities of science, education, and efficacy,” he said.
During the action-packed opening ceremony, there were also a number of awards presented to respiratory health individuals who had distinguished themselves in their respective specialisms. Firstly, Prof Luigi Allegra, regarded as one of the founding fathers of the ERS, received the ERS Congress Chair Award for his contributions to research and training in the area of lung disorders, as well as his commitment to the care of patients with such conditions. The ERS Presidential Award went to Dr Sally Wenzel, who was recognised for the pioneering work and exceptional contributions she has made to the field of asthma.
Next, the ERS Gold Medal was given to three researchers for making an outstanding contribution to their respective fields of asthma, chronic obstructive pulmonary disease, and idiopathic pulmonary fibrosis. The recipients of the prizes (and €50,000 each) were Dr Bart Lambrecht, Dr MeiLan Han, and Prof Vincent Cottin. The orator of this year’s Sadoul lecture, which honours senior scientists of great standing, was Dr Dirkje S. Postma, and was delivered on Sunday 10th September. Prof Stefano Nava then accepted the ERS Educational Award for his contribution to respiratory education. Following this, the Chair of the European Lung Foundation (ELF), Mr Dan Smyth, came on stage to hand the 2017 ELF Award to Prof Colin Sullivan for his work in improving the lives of patients with sleep apnoea. These were just some of the awards bestowed at the 2017 ERS congress, highlighting the impressive work and advances taking place within the field.
As always, there was a tremendous amount of research presented throughout the 5 days of the congress, enhancing knowledge and displaying the new treatment options that have recently emerged for the many types of respiratory conditions that exist, using some innovative methods to spread the messages as far as possible. For example, live sessions were streamed to other continents, including to Latin America for the first time. It was a truly ground-breaking congress and we hope this theme continues at next year’s ERS annual meeting, which will be held in Paris, France.

Asthma Symptoms Potentially Reduced by Park Access
DISTANCE to the nearest park has been correlated with the number of days children with asthma who live in the city present with asthma symptoms, according to results presented at the ERS congress and reported in a ERS press release dated 8th September 2017. It was found that the closer children lived to a park, the fewer asthma symptom days (ASD) they tended to have. This Baltimore-based study (Maryland, USA) enrolled 196 children, the majority of whom were male (66%), African American (95%), and Medicaid insured (95%), which meant they were from a population at high risk of asthma-related mortality. The children had a mean age of 6.4 years. The home address of each child was noted and then marked on a map of Baltimore that featured the locations of city parks. This geocoded map was then used to calculate the distance to the closest park, and it was found that the mean distance to the closest park was 826 ft.
ASD were assessed by means of questioning the child’s primary caregiver on the number of days their child had presented with symptoms such as chest pain, wheezing, and shortness of breath. The researchers conducted a multivariate analysis to model ASD against park distance and discerned that there was a significant association between a shorter distance to the nearest park and a reduced number of ASD (standardised β=0.15; p=0.042). This corresponded to one extra ASD for every additional 305 m from the park; a child who lived next door to a park had 5 ASD on average, whereas a child whose home was 305 m away had an average of 6 ASD. Drilling down into the data further, a stronger association was found for children aged 6–12 years compared with those aged 3–5 years (standardised β=0.32; p=0.002). The researchers speculated that the reason for this was because older children had more freedom to choose where they wanted to go and hence were more likely to take advantage of their proximity to local green space. In the 6–12 years old group, a multivariate analysis was conducted to control for second-hand smoke exposure and short-acting beta agonist use. It was found that distance to park remained independently associated with ASD (standardised β=0.30; p=0.003).
The researchers hoped that their research would be taken into account by urban planners and that it would lead to additional city parks. Commenting further on the findings, the study’s presenter, Kelli DePriest, Johns Hopkins University School of Nursing and Medicine, Baltimore, Maryland, USA, also suggested they should be considered by healthcare providers. She pronounced: “They will also help healthcare providers to take a more holistic view of their patients by understanding how access to green space might affect health.” Looking to the future, there are plans to further explore the relationship between green space and asthma symptoms by considering different types of green space, such as gardens.
Respiratory Infections Linked with Asthma and Lung Function
RISK of both asthma and decreased lung function in later life is increased with respiratory tract infections in early life. These results, from the Generation R Study Group at Erasmus MC University Medical Centre, Rotterdam, Netherlands, were presented at the ERS congress 2017, and reported in a ERS press release dated 10th September 2017. Asthma and lung function are two different respiratory measures that are not necessarily fully related. Lung function is a measure of an individual’s ability to breathe, usually determined using a spirometer, which measures forced viral capacity (FVC), forced expiratory volume in one second (FEV1), and forced expiratory flow at 75% of FVC (FEF75). On the other hand, asthma is a condition characterised by spasms of the bronchi in the lungs and may not greatly affect lung function.
The meta-analysis included 154,942 children from across Europe for whom data were available regarding respiratory tract infections (RTI) from 6 months to 5 years of age, lung function, and/or asthma. Lung function was monitored using a spirometer as the children grew older. The study included both upper RTI as well as lower RTI. The results highlighted that the presence of an upper RTI was not associated with worsened lung function, but the children had a 1.5-fold increased risk of developing asthma. The presence of a lower RTI, however, was associated with worsened lung function, with lower FVC, FEV1, and FEF75 scores, and also resulted in a two-to-four-fold increased risk of asthma.
Dr Evelien van Meel, Erasmus MC University Medical Centre, concluded: “These findings support the hypothesis that early-life respiratory tract infections may influence the development of respiratory illnesses in the longer term,” but went on to say: “However, at this stage we cannot say for certain whether the relationship is causal.” The researchers hope to perform future studies that determine the percentage of associations between RTI and asthma, which can be explained by lung function changes, including whether these associations alter when considering early life wheezing. They also hope to analyse how paracetamol, antibiotics, and second-hand smoke exposure affect these relationships.

Asthmatic Children More Likely to be Prescribed Unnecessary Antibiotics
CHILDREN with asthma are more likely to be prescribed antibiotics compared to non-asthmatic children, even if there is no symptomatic evidence that they need them, according to a multi-national study presented at the ERS 2017 congress and reported in a ERS press release dated 11th September 2017.
It has been well publicised that the overuse and misuse of antibiotics leads to a rise in difficult-to-treat infections. Dr Esmé Baan, Department of Medical Informatics, Erasmus University, Rotterdam, Netherlands, explained that asthmatic children already face day-to-day difficulties, such as not being able to play with their peers and having to take days off school. Dr Baan went on to comment: “We do not want to compound this with prescribing drugs that will not help and may be harmful.”
The study consisted of 1.5 million (including around 150,000 with asthma) and 375,000 (including around 30,000 with asthma) children from the UK and the Netherlands, respectively. The Netherlands and the UK both follow the same international guidelines on asthma treatment; however, antibiotic prescriptions were twice as common in the UK compared to the Netherlands. Researchers also found that children with asthma were approximately 1.6-times more likely to be prescribed antibiotics compared to those without asthma.
On an annual basis, per 1,000 children with asthma, 374 and 197 were prescribed antibiotics from the UK and the Netherlands, respectively, compared to 250 and 126 non-asthmatic children, respectively. With the trend for prescribing antibiotics to asthmatic children being so similar between the two countries, the researchers believed that this trend may also be similar in other countries. The Netherlands prescribes some of the lowest numbers of antibiotics in the world and, as such, the researchers expressed concern that the situation in countries where antibiotics are prescribed more frequently, such as Italy, Spain, Portugal, and Greece, could be worse.
Dr Baan explained: “Antibiotics should only be given when there is clear evidence of a bacterial infection, such as for pneumonia. However, we saw that, in children with asthma, most of the antibiotic prescriptions in children were intended for asthma exacerbations or bronchitis, which are often caused by a virus rather than bacteria.” Dr Baan acknowledged: “It can be difficult for a general practitioner (GP) to differentiate between a deterioration in asthma symptoms and a bacterial respiratory infection,” and this was the reason why researchers believed asthmatic children are being overprescribed antibiotics. Dr Baan concluded by noting that sometimes antibiotics are genuinely needed, but discouraged doctors from prescribing unnecessary antibiotics, in order to reduce the risk of drug-resistant infections.
Nicotine-containing E-cigarettes Linked to Arterial Stiffness
PRELIMINARY results from a recent study have shown that the use of nicotine-containing e-cigarettes leads to arterial stiffening in healthy volunteers, heightening the risk of cardiovascular disease. With numbers of e-cigarette users soaring, the implications of the study are vital for understanding the possible adverse effects of the smoking substitutes, which are often marketed as less harmful than traditional cigarettes.
A ERS press release dated 11th September 2017 reported the study, which was conducted by Dr Magnus Lundbäck, Department of Clinical Sciences, Danderyd Hospital, Karolinska Institute, Stockholm, Sweden. Dr Lundbäck and colleagues randomised 15 healthy, young volunteers to use e-cigarettes with or without nicotine for 30 minutes on alternate days. The volunteers were noted to be seldom smokers, not smoking >10 cigarettes per month, and none of them had used e-cigarettes prior to the study. The volunteers’ average age was 26 years; 59% of volunteers were female. Blood pressure, heart rate, and arterial stiffness were all measured immediately after smoking, and then again 2 hours and 4 hours later. The team noted that volunteers who had smoked nicotine-containing e-cigarettes demonstrated a significant increase in blood pressure, heart rate, and arterial stiffness in the 30 minutes immediately following smoking. Volunteers who smoked e-cigarettes without nicotine, however, were not affected in this way.
Commenting on the sharp spike in heart rate, blood pressure, and arterial stiffness, Dr Lundbäck stated: “It is very important that the results of this and other studies reach the general public and the health care professionals working in preventive health care, for example in smoking cessation. Our results underline the necessity of maintaining a critical and cautious attitude towards e-cigarettes, especially for health care professionals,” adding: “The marketing campaigns of the e-cigarettes industry target current cigarette smokers and offer a product for smoking cessation. However, several studies question the e-cigarette as a means of smoking cessation, and there is a high risk of double use, where people use both e-cigarettes and conventional cigarettes. Furthermore, the e-cigarette industry also targets non-smokers, with designs and flavours that appeal to a large crowd.”
Dr Lundbäck concluded: “Therefore, our research concerns a very large population and our results may prevent future health problems for a huge number of people. It is of the utmost importance to investigate further the possible long-term effects of daily e-cigarette use through studies that are funded independently of the e-cigarette industry.”
Potential Risks of E-Cigarettes
AN EXAMINATION of e-cigarettes and their usage has revealed potentially associated risks, according to the results of two studies recently presented at the ERS congress, as reported in a ERS press release dated 11th September 2017. It was also suggested that these risks were heightened if e-cigarette usage was combined with the smoking of conventional cigarettes. It is hoped that these studies will provide some measure of guidance to doctors and the users of e-cigarettes.
The first study examined the content of e-cigarette refills. The researchers picked a random sample of the most popular e-cigarette brands across nine European countries, including the UK, Spain, Romania, Poland, Hungary, and Germany. This resulted in a selection of 122 liquids that were analysed to determine their chemical composition and their respective quantities. Every one of the 122 liquids tested was found to contain at least one substance that the United Nations (UN) classification system identified as presenting some level of risk to health. For instance, 26.3% of samples contained methyl cyclopentanolone and 8.7% contained α-ionone. The classification of both of these substances indicates that they “may cause allergy or asthma symptoms or breathing difficulties if inhaled.” Furthermore, there were several substances found that were classified as: “able to cause respiratory irritation.” These included menthol (42.9% of samples), ethyl vanillin (16.5%), and acetyl pyrazine (8.2%).
Commenting on the findings of this study, the lead author, Dr Constantine Vardavas, University of Crete, Crete, Greece, declared: “Based on this work, we also think users should be aware that e-cigarettes are not risk-free and that doctors should inform their patients that e-cigarettes may contain respiratory irritants.” He also commented that there is currently limited information available on the influence that the components of e-cigarette liquids may have on respiratory health, which represents an area for further consideration in the future.
The second study presented at the ERS congress surveyed >30,000 individuals residing in Sweden. The questionnaire was designed to obtain information on their smoking habits, including the use of e-cigarettes, and respiratory symptoms. The breakdown of results showed that 11% of respondents smoked purely conventional cigarettes, 0.6% smoked only e-cigarettes, and 1.2% smoked both conventional and e-cigarettes. Upon examining the reported respiratory symptoms, it was revealed that the 1.2% of individuals who smoked both types of cigarette were the most likely to present with respiratory symptoms. Indeed, 56% of dual users reported respiratory symptoms. This compared with 46% of conventional cigarette smokers, 34% of e-cigarette smokers, and 26% of non-smokers (p<0.001).
The researchers added the caveat that the results did not prove that dual usage was responsible for increased incidence of respiratory symptoms. For instance, it was noted that smokers currently presenting with respiratory symptoms might be concurrently using e-cigarettes as part of a smoking cessation process. More studies are needed to establish the impact of e-cigarettes on respiratory health, although the results of these two studies contribute to the growing body of evidence that e-cigarettes should not be marketed as a safe alternative to conventional cigarettes.

Second-hand Smoke Exposure Increased in Workplaces Around Europe
INCREASED numbers of individuals who work indoors are exposed to second-hand smoke at work, despite widespread smoking bans, according to new findings presented at the ERS congress 2017 and reported in a ERS press release dated 9th September 2017. New no-smoking laws have been enforced in several countries throughout the European Union (EU), but some countries are better at enforcing these laws than others. The bans came about following numerous research projects that established the risks of second- hand smoke exposure, including progression to coronary heart disease, stroke, and lung cancer, with a combined responsibility for >600,000 deaths around the world each year.
A survey including >55,000 people from within the EU formed the basis of the study. Approximately half of these people completed the study in 2009, with the remaining half in 2014. The results found that in 2014, 25.1% of respondents were exposed to second-hand smoke in bars, compared to 45.1% of respondents in 2009, a significant decrease. Following the same trend, 11.8% of respondents were exposed to second-hand smoke in restaurants in 2014, compared to 30.2% in 2009. In contrast, 27.5% of respondents were exposed to second-hand smoke within their workplace in 2014, compared to 23.8% of respondents in 2009. The researchers suggest that these results are due to difficulties in regard to complaints being made in the workplace, as well as major differences in the levels of legislation enforcement between different countries. Dr Filippos Filippidis, Imperial College London, London, UK, said: “Our results suggest there is still a lot more work to be done to protect people in some parts of Europe.” He further explained: “This research is an essential way for us to monitor the progress that EU countries are making in upholding smoke-free laws.”
The researchers aim to continue their research on second-hand smoke exposure around Europe, with efforts being made to determine why some countries do not enforce legislations as well as others. Once these results are established, better legislation can be encouraged, ultimately reducing second-hand smoke exposure and providing a huge step forward for public health.
Regular Use of Disinfectant is Associated with COPD
NURSES who regularly use disinfectants for tasks, such as cleaning surfaces, are at a higher risk of developing chronic obstructive pulmonary disease (COPD), according to a study presented at the ERS 2017 congress and reported in a ERS press release dated 11th September 2017. The study analysed data from 55,185 female registered nurses enrolled in the US Nurses’ Health Study II, initiated in 1989. Dr Orianne Dumas, INSERM, Villejuif, France, and colleagues studied practising nurses who had no prior history of COPD from 2009 until May 2017. A questionnaire was used to evaluate disinfectant exposure, as well as a matrix that assigned exposure to disinfectants by job or task. The data were adjusted for smoking habits, age, BMI, and ethnicity.
During the 8-year study period, 663 nurses were diagnosed with COPD. Dr Dumas commented on the results, saying: “We found that nurses who use disinfectants to clean surfaces on a regular basis, at least once a week, had a 22% increased risk of developing COPD.” Researchers also assessed different types of disinfectant and their relationship with COPD risk, including glutaraldehyde (for medical instruments), bleach, hydrogen peroxide, alcohol, and quaternary ammonium compounds (for floors and surfaces). The increased risk of COPD ranged from 24–32% (p<0.05). Of the study population, 37% used disinfectants to clean surfaces and 19% cleaned medical instruments with disinfectant on a weekly basis.
The affect disinfectants have on asthma among healthcare workers has been well documented, but there has been significantly less consideration on COPD risk. Dr Dumas commented: “To the best of our knowledge, we are the first to report a link between disinfectants and COPD among healthcare workers, and to investigate specific chemicals that may underlie this association.” She went on to say: “These are preliminary findings and more research needs to be carried out. In particular, we need to investigate the impact on COPD of lifetime occupational exposure to chemicals and clarify the role of each specific disinfectant.” Dr Dumas emphasised that these results are only observational and provide only an associated risk at this stage. Further research is required to assess the lifelong exposure risk and to understand whether this correlation is, in fact, a causational link. It is hoped that these findings will be utilised in the development of updated guidelines on cleaning and disinfection in healthcare settings that take into account the potential associated risks.

Effects of Asthma on Fertility Investigated
A SERIES of studies have analysed the association of asthma and fertility, a ERS press release dated 12th September 2017 has reported. The studies, carried out in Denmark and Australia, looked at the association between asthma diagnoses and time to pregnancy, and the link between maternal e-cigarette vaping and offspring risk of allergic asthma, respectively.
In the study from Denmark, 744 pregnant women were enrolled in the study at Hvidovre Hospital, Hvidovre, Denmark. Eligibility criteria included: i) a diagnosis of asthma, ii) had their first visit to the respiratory clinic in the first 18 weeks of pregnancy, and iii) had given birth between 2007 and 2013. Each participant under these criteria was studied alongside three consecutive non-asthmatic women who gave birth at the same hospital. The average age in the asthmatic and control groups was 31.3 years (range: 17–44) and 30.9 years (range: 17–45), respectively. Results were adjusted to account for differences in age, BMI, smoking status, previous children, and relationship status; however, it was noted that there were possible differences in income, lifestyle, and socioeconomic status. It was also noted whether the births were the result of spontaneous conception, or whether the mother had undergone assisted reproductive therapy, such as in vitro fertilisation (IVF), or intrauterine insemination. The team found that 12% of the asthmatic women had undergone fertility treatment compared to 7% of the control group participants.
Prof Charlotte Suppli Ulrik, Department of Respiratory Medicine, Hvidovre Hospital, Hvidovre, Denmark, commented: “We don’t have the hard-core evidence, but based on what we know, it seems very likely that good asthma control will improve fertility in women with asthma by reducing the time it takes to become pregnant and, therefore, the need for fertility treatment.” Following these results, Prof Suppli Ulrik and colleagues are now hoping to further study this association and to assess the effects of effective asthma control on fertility.
The second study to be presented looked at maternal e-cigarette vaping and the risk of allergic asthma in offspring by exposing female mice to vapour both with and without nicotine, and normal room air prior to mating and during gestation and lactation.
Following this, offspring were exposed to an ovalbumin-based allergen in order to develop asthma. Additionally, the team exposed in vitro human cells to e-cigarette liquid of a range of concentrations and assessed mitochondrial function.
Commenting on the results of the study, Dr Pawan Sharma, University of Technology, Sydney, Australia, explained: “Our study found that maternal vaping increased the risk and severity of allergic asthma in offspring. We also found that the detrimental effects of vaping were partially mediated through impairment of mitochondrial function, which affects cellular respiration, and were independent of nicotine. This means that vaping, even without nicotine present, has a demonstrated negative impact on cell function.”
Hormone Replacement Therapy for Preservation of Lung Function
AN INHIBITION of the decline of lung function in middle-aged women can be achieved by the use of hormone replacement therapy (HRT) as a therapeutic option, according to research recently presented at the ERS congress and reported in a ERS press release dated 12th September 2017. Lung function begins to decline after people reach their mid-twenties. Currently, a variety of factors are known to influence the speed of this decline, with the menopause having been identified as an accelerating factor.
In this research, data was used from the European Community Respiratory Health Survey, which followed 3,714 women for a period of approximately 20 years up to 2010. When the women initially joined the survey, they had their lung function assessed by measurement of forced vital capacity (FVC). This measurement was repeated 20 years later.
In this study, the researchers identified 236 women who took long-term HRT, which was defined as ≥2 years of treatment, and then matched them by characteristics including age at menopause, smoking behaviour, age, weight, height, and baseline lung function, with 236 women who had never undergone HRT. After adjusting for additional factors, such as length of follow-up time and type of spirometer, it was found that, over the study’s duration, the women in the long-term HRT group had lost an average of 46 mL less lung volume when compared to the women in the control group. It was noted that 46 mL was approximately the lung volume that would be lost if a woman smoked a pack of cigarettes every day for 3 years; however, the researchers were at pains to point out that HRT should not be a substitute for quitting smoking.
Dr Kai Triebner, University of Bergen, Bergen, Norway, announced the headline discovery: “Our findings show that female sex hormones are important for the preservation of lung function in middle-aged women.” However, when placing the results of their study into a holistic health context, the researchers discussed some of the other health impacts associated with HRT: it has a protective effect against osteoporosis and can alleviate menopausal symptoms but, on the other hand, has also been associated with increased risk of breast cancer and heart and blood vessel problems. Therefore, this finding should form part of a personalised treatment approach for women going through the menopausal transition, as the exact therapeutic option will depend on the individual situation and risk factors.
Lifestyle Changes Improve Asthma Symptoms in Non-Obese Patients
DIETARY and exercise changes could positively affect quality of life and symptoms in non-obese asthma patients, as shown by new research presented at the ERS congress 2017 and reported in a ERS press release dated 13th September 2017. As asthma is a relatively common condition, affecting approximately one-in-ten individuals in the Western world on a long-term basis, new developments in management are important. Currently, daily medicine is the main method of controlling symptoms, with patients usually reluctant to participate in exercise for fears of exacerbating their symptoms.
The study randomly assigned 149 patients into four groups: i) consumption of a high protein diet with a low glycaemic index (to maintain blood sugar levels) and at least six portions of fruit and vegetables each day, ii) participation in three exercise classes at hospital per week, including both high intensity activities to increase the heart rate and more relaxed activities, iii) combination of the above diet and exercise programmes, and iv) a control group involving none of the above. The study lasted 8 weeks, with 125 patients completing the full study duration. Patients were questioned regarding their symptoms, quality of life, fitness level, strength, and lung capacity.
The study deemed high intensity exercise safe for asthma patients. There was no definite improvement in patient lung function; however, the combination of the diet and exercise allowed better patient control of symptoms and improved quality of life and fitness levels. Patients in the combination diet and exercise group defined their asthma symptom score as 50% better on average than those in the control group. Although patients in the individual diet and exercise groups also rated their scores higher than the control group, (by an average of 30%), these results were not found to be statistically significant. Dr Louise Lindhardt Toennesen, Bispebjerg University Hospital, Copenhagen, Denmark, stated: “Our research suggests that people with asthma should be encouraged to eat a healthy diet and to take part in physical activity.” Future research will investigate these results in the long-term. The researchers hope to establish particular diets and exercises that have the best outcome for asthma symptoms, with the ultimate aim of replacing daily asthma medicine with improved diet and increased exercise.








