The ‘City of Peace’, Paris, France, played host to this year’s European Respiratory Society (ERS) International Congress. With the nation bringing forth science, architecture, fashion, and food, the French capital city was the perfect place to celebrate the previous year’s records and achievements while also looking to the future, having had “some of the most significant scientific and medical breakthroughs in human history,” as stated in this year’s opening ceremony.
The opening ceremony welcomed delegates from all over the world to the sound of romantic music: the perfect tribute to the choice of location. France’s historical achievements were acknowledged with pride in the initial introduction, one of which included the use of the first gasoline-powered taxi in Paris in 1899. The French motto: “Liberté, égalité, fraternité,” which translates as “liberty, equality, fraternity,” was reiterated and celebrated not only in the opening ceremony but throughout the event. The motto originated during the French revolution, which brought about the “Declaration of the Rights of the Man” in 1789, a crucial human civil rights document that would later inspire the Universal Declaration of Human Rights.
Prof Mina Gaga, President of the ERS, then took to the stage to pay her respects to the ERS and the success of the previous year. With increased membership, well-attended events, and new strategies for the society being brought into place, the future is looking bright. Prof Gaga noted that the world is changing and, as such, the society and the ERS Congress must change with it. One of these changes includes creating a congress that is more accessible and relevant for patients: “Patients help us share our thoughts about the disease and think that there is always something we can do even if we do not have hope, and so it is so important to include our patients,” she said. “We are here for the patient, we are here for the people.”
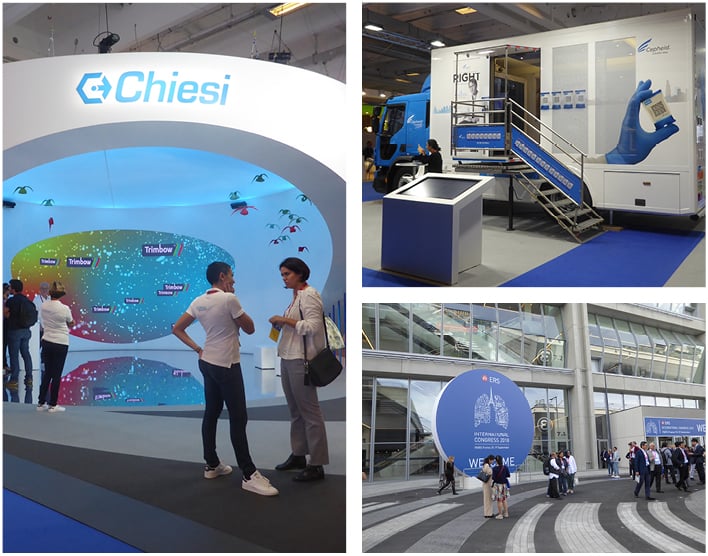
The involvement of patients at the congress included the addition of the European Lung Foundation (ELF) Patient organisation programme. Working tirelessly to bring patients and the public together with respiratory professionals, the organisers of the ELF Patient organisation programme created the World Village at the ERS Congress, a project that brought together patient organisations from all over the world. The activities involved a variety of respiratory diseases for attendees to delve into, focussing on networking, building and strengthening partnerships, and sharing knowledge about future activities around the globe.
Finishing her opening ceremony speech, Prof Gaga encouraged attendees to “network, learn, teach, and be with friends,” before acknowledging the achievements of the most esteemed healthcare professionals by presenting them with awards for their significant contributions to the world of respiratory medicine, including the special ERS Gold Medals.
As the opening ceremony came to a close and the congress was officially in full-swing, attendees reflected on the wonders that were announced and waited in anticipation of what the congress had to offer. Brand new to the ERS Congress was the “Therapeutic breakthroughs: Year in review” session, which covered paediatrics, allied healthcare professionals, thoracic oncology, and respiratory intensive care. This session was a fantastic opportunity for attendees to discuss the most significant therapeutic advances of the last year within these varied fields.
In addition, the “Lungs on Fire” session formed another brand-new event with a twist. This interactive session allowed the audience to diagnose clinical cases with a panel of experts. Multiple choice questions were presented to audience members throughout the session, which consisted of a single moderator in the room with details of each case. This wonderful experience gave attendees the opportunity to challenge themselves with real clinical cases and was perfect for learning and exchanging thoughts and ideas.
With the latest updates, collaborations, and research galore, attendees found themselves, as always, in awe of this imperious event. We look forward to seeing you all at next year’s ERS Congress, which heads south to Madrid, Spain.
Access to Green Space During Childhood is Beneficial for Lung Health
RESPIRATORY PROBLEMS, such as asthma and wheezing, are less likely to be experienced by adults if they had access to green space close to their childhood homes. Reported in a ERS press release dated 19th September 2018, the preliminary results of the RHINESSA study indicate the long-term effects of exposure to air pollution on respiratory health.
In a new analysis of lung health in children and adults from seven European countries, green space data from 5,415 individuals aged between 18 and 52 years were investigated, as well as information on air pollution from 4,414 participants. Average annual exposure to particulate matter (PM2.5 and PM10) and nitrogen dioxide, in addition to ‘greenness’ in a 100 m zone around the home (as assessed by the Normalised Difference Vegetation Index), were calculated for the participants from birth until 18 years of age.
When looking at the number of study individuals who experienced reduced lung health, 12.0% had >3 respiratory symptoms, 7.7% had severe wheeze, and 9.4% experienced late-onset asthma. Analysing the data further, PM2.5 and nitric oxide increased the probability of late-onset asthma by 6–22% in Bergen, Norway, while exposure to green space at <10 years of age correlated with a 71% lower probability of experiencing wheeze in adults in Tartu, Estonia. Although further analysis is required, the researchers noted that the results showed that exposure to green space during childhood was associated with fewer respiratory problems later in life.
As well as allowing physicians to gain a greater understanding of the importance of childhood exposure to air pollution and access to green space, these findings may also impact broader public health and societal regulations. “We believe that our results, seen together with previous results, will be of particular value for city planners and policy-makers,” commented Dr Ingrid Nordeide Kuiper, Haukeland University Hospital, Bergen, Norway. When highlighting the implications of these findings for the future of respiratory disease management and prevention, Prof Mina Gaga, President of the ERS, commented: “The ongoing work of the RHINESSA study will, no doubt, produce more interesting and useful results to support these early indications.”
Trained Artificial Intelligence More Accurate at Diagnosing Lung Disease Than Pulmonologists
ARTIFICIAL INTELLIGENCE (AI) is increasingly set to revolutionise the modern world across a host of industries and this is certainly true for the field of medicine. New research has demonstrated that a pulmonologist-trained AI programme could outperform human medical practitioners alone when it comes to diagnosing lung disease, as reported in a ERS press release dated 19th September 2018.
A panel of pulmonologists used the results of pulmonary function tests (PFT), which included spirometry, a body box or plethysmography test, and a diffusion capacity test, as well as the respective medical history of 1,430 patients to arrive at an agreed correct diagnosis for each patient; these diagnoses were measured against gold standard guidelines from the European Respiratory Society (ERS) and American Thoracic Society (ATS). These correct diagnoses and their component factors were then used to ‘train’ the AI programme, with the hope that it would be able to subsequently identify patterns in the training data to correctly diagnose new patients. “When training the AI algorithm, the use of good quality data is of utmost importance,” explained Dr Marko Topalovic, Catholic University of Leuven, Leuven, Belgium.
The AI programme was then compared to 120 pulmonologists from 16 European hospitals; both the AI programme and medical professionals received PFT data from 50 randomly selected patients from which to make a diagnosis, measured against gold standard guidelines, as before. The results showed the pulmonologists’ diagnoses matched the guidelines in 74% of cases, while the AI’s matched in 100% of cases; the correct primary disease was diagnosed in 45% and 82% of cases, respectively.
The researchers were quick to stress that pulmonologists have a broader perspective of each case, since they are working from more than just PFT, and thus are able to diagnose based on a greater number of factors. Dr Topalovic explained: “These results show how AI can serve as a second opinion in pulmonologists when they are assessing and diagnosing their patients.”
Besides further studies, the next key step in this process will be using the AI technology in primary care, where general practitioners can use the resulting data to make the correct diagnostic decision.
Targeted Lung Denervation Significantly Improves COPD Patient Health
OPENING obstructed airways of chronic obstructive pulmonary disease (COPD) patients via targeted lung denervation (TLD) can safely reduce respiratory problems associated with the disease. With 4–10% of European adults affected by COPD, these significant results, reported in a ERS press release dated 18th September 2018, will have important implications for patient quality of life and healthcare costs.
TLD involves the delivery of radiofrequency energy to the airways, causing them to relax and widen and decreasing inflammation and mucus production. To investigate the use of TLD in combination with tiotropium, a commonly used anti-cholinergic bronchodilator, the double-blind AIRFLOW 2 Phase II trial randomised patients to receive either the airway opening procedure or a sham procedure.
Presented at the ERS Congress, initial results based on 82 patients (50% male; average age: 64 years) showed that there was a positive benefit of TLD treatment over sham procedure. After 3–6 months of treatment, 71% of sham procedure patients, who did not receive the electrical radiofrequency charge, experienced adverse respiratory events related to COPD, compared to 32% of TLD treatment patients. Furthermore, a >50% reduction in the number of patients hospitalised for respiratory conditions was shown in the treatment arm versus the sham group. As well as being shown to effectively improve respiratory health, TLD was also proven to be acceptably safe, with no TLD-related adverse side effects that required treatment reported and only 5 patients experiencing temporary gastrointestinal effects.
Proudly discussing his team’s results at the congress, Dr Dirk-Jan Slebos, University Medical Centre Groningen, Groningen, Netherlands, commented on the implications of TLD for COPD patients: “It offers the ability to significantly reduce symptoms and exacerbations even in patients already on aggressive medical therapy.” AIRFLOW 3, a larger Phase III trial, is now in development and will include many more patients to significantly improve COPD patient health. “Better treatments for COPD patients, particularly those with severe disease, are desperately needed and we look forward to the results from the AIRFLOW 3 trial, which we hope will confirm this [TLD] as an effective and safe treatment,” commented Prof Daiana Stolz, Chair of the ERS Education Council.
Simple Test Accurately Diagnoses Viral Infections in 50 Minutes
FIFTY minutes is all it takes to diagnose a viral infection using a new test developed by researchers at West Hertfordshire Hospitals NHS Trust, Watford, UK and the University of Hertfordshire, Hatfield, UK. This test, as reported in a ERS press release dated 17th September 2018, could greatly reduce unnecessary hospital admissions and antibiotic prescriptions.
The new service, called point of care respiratory viral testing (POCT), involves swabbing the back of the nostril to collect secretions and inserting the prepared sample into a compact machine called a FilmArray®, which analyses the sample; the entire process is estimated to take around 50 minutes. “The whole process from obtaining a sample from the patient’s nose to getting a result should take under 50 minutes, which has a potentially enormous impact on quality of care, improving the patient journey by allowing earlier, informed decision-making about patient management,” explained Dr Kay Roy, University of Hertfordshire. This short diagnostic process represents a huge improvement on similar tests using the same technology that would take 2 days to process in a microbiology lab.
Initial experiences using POCT alongside other diagnostic techniques (such as chest X-ray) have been very positive; of the first 1,075 patients to take the test, 121 were identified as having viral infections, had no evidence of bacterial infection, had normal X-ray results, and had only modest indicators of inflammation. As a result, hospital admission was avoided in 25% of this group, and antibiotic prescription was avoided in 50%; none of the patients in either of these subgroups experienced adverse clinical outcomes. Most of the viral infections diagnosed were influenza (56%), with the remaining viruses including rhinovirus, coronavirus, metapneumovirus, and adenovirus.
Diagnosing these infections early could save healthcare providers thousands in unnecessary hospital admissions and antibiotic prescriptions. “Each respiratory admission can cost around £2,000,” explained Dr Roy. “We could make a significant saving for national health services by avoiding unnecessary admissions in patients who may have been otherwise admitted and given antibiotics while waiting up to 2 days for results from the lab.”
A randomised controlled trial is now being planned wherein general practitioners will be able to refer patients to a community hub for POCT.
Paracetamol Use Linked to Increased Asthma Risk
TAKING paracetamol in the first 2 years of life has been linked to an increased risk of asthma in teenagers, according to new research from the University of Melbourne, Melbourne, Australia, which was presented in a ERS press release dated 17th September 2018.
The research found that the link between paracetamol use and asthma was strongest among those who had certain genetic makeups, specifically a variant of the glutathione S-transferase (GST) gene, GSTP1. In addition, another GST gene variant, GSTM1, was found to be linked with reduced lung function.
GST genes code for enzymes that use an antioxidant called glutathione, which is responsible for clearing the effects of toxins around the body and lungs. In doing so, glutathione helps to prevent inflammation and damage to cells. It is known that paracetamol removes glutathione from the body, stopping the beneficial effects it has in preventing damage and inflammation. The researchers hypothesised that those individuals with certain genetic variations or deletions who, as a result, did not have full GST enzyme activity, were more at risk of adverse effects on the lung due to paracetamol use.
The study included 620 children who were chosen based on being potentially at a higher risk of developing an allergy-related disease. The children were followed from birth until they were 18 years old, as part of the Melbourne Atopy Cohort Study. Every 4 weeks for the first 15 months of life, and then again at 18 months, a research nurse rang the family of the child to ask how many days in that period the child had taken paracetamol. At 18 years old, the participants were asked to give a sample of blood or saliva to test for the genetic variants GSTT1, GSTM1, and GSTP1. In addition, the participants were tested for asthma and underwent a spirometry test to assess air inhalation and exhalation when breathing through a mouthpiece.
It was found that the GSTP1 Ile/Ile variant was associated with a 1.8-fold increased risk of developing asthma by the age of 18 years for each doubling of the days receiving paracetamol when compared to those who had less paracetamol. However, it was also noted that those children with other types of GSTP1 receiving paracetamol did not have any altered level of risk. In addition, those children who had a dysfunctional version of GSTM1 had a small but significant reduction in the amount of air they could breathe out in 1 second.
It is worth mentioning that this link may not necessarily be a result of paracetamol but may rather be a result of viral lower respiratory tract infections in the first 2 years of life that had been treated with paracetamol. The researchers emphasised that further research must be carried out to affirm these results and to determine what is best for patients. “As we learn more about the genes involved in asthma, and how they interact with the environment and the medicines we use, we hope to learn more about what is best for individual patients,” said Prof Guy Brusselle, Chair of the ERS council, when commenting on the results.
Air Pollution and Pregnancy: A Greater Understanding
CARBON PARTICLES have been found in placentas for the first time, suggesting that components of polluted air can directly impact a growing fetus via the mother’s blood. This new research, revealed at the ERS Congress and reported in a ERS press release dated 16th September 2018, will lead to increased public awareness of the harmful effects of air pollution for pregnant women and ensure appropriate management of air quality.
It has long been known that exposure to air pollution during pregnancy can have a direct impact on adverse birth effects, such as low birth weight, premature birth, and infant mortality, as well as long-term child and adulthood development. “We were interested to see if these effects could be due to pollution particles moving from the mother’s lungs to the placenta. Until now, there has been very little evidence that inhaled particles get into the blood from the lung,” commented Dr Lisa Miyashita, Queen Mary University of London, London, UK.
Led by Prof Jonathan Grigg, Queen Mary University of London, the research group studied the placentas of five women who had uncomplicated pregnancies and gave birth to healthy babies. A total of 3,500 placental macrophages were examined for carbon particles and 72 small black areas across 60 cells were found. This equated to an average of approximately 5 μm2 of black on each placenta, which was believed, following electron microscopy, to be composed of tiny carbon particles.
Drawing upon the results of previous research showing that these sooty particles are present in macrophages in the airways, the team concluded that the identification of carbon in the placenta indicated that inhaled pollution particles can move from the lungs into the circulation and then into the placenta. While it is still uncertain if the particles can be transferred to the fetus, this research suggests a possible mechanism by which unborn babies are affected by air pollution exposure. Stricter policies for cleaner air are therefore recommended to improve health worldwide.

Re-Evaluating the Impact of Childhood Asthma on Adult Life
CHILDHOOD asthma may greatly impact later life, both academically and professionally, suggests new research from Karolinska University Hospital, Stockholm, Sweden, presented in a ERS press release dated 16th September 2018. While the impact of asthma on quality of life is well established, its consequential effects on later life remain unclear, prompting this important study.
In 1996, children aged 7–8 years old from three Swedish districts were invited to participate in the study, with 97% agreement. Follow-ups were conducted at 11–12, 19, and 27–28 years of age, and 59% of participants (n=2,291) were still being studied as of 2015.
The children were assessed for asthma at each follow-up and also the age at which they left education, what their occupation was, and other factors, such as sex, weight, and smoker status. An analysis of this group revealed that those with early-onset asthma (here defined as asthma diagnosed before the age of 12 years that was still present at 19 years) were 3.5-fold more likely to leave school at 16 years than those without asthma, as well as being twice as likely to drop out of university before completing a 3-year course. This group also had a noticeable detriment to their careers, being >50% less likely to enter occupations such as being a police officer, a musician, or a nursing assistant.
The reason for this considerable impact is, at present, unclear, but researchers suggested that asthma may impact school attendance and drive people away from certain professions that may require stamina or could trigger their asthma. “Until we know more about exactly why childhood asthma affects education and job prospects, the key message for families is to try and ensure children stick to their asthma treatments and to speak to a doctor if symptoms are not under control,” explained Dr Christian Schyllert, Karolinska University Hospital.
The researchers intend to continue to follow this study cohort for a further decade, as well as examining another group 10 years younger to compare the effects between cohorts.
Developing Asthma in Adulthood Associated with Higher Risk of Obesity
ACCORDING to a ERS press release dated 15th September 2018, in addition to obesity being a known risk factor for developing asthma, people with asthma have now been identified as being at an increased risk of becoming obese, suggests research conducted as part of the European Community Respiratory Health Survey.
A total of 8,618 people from 12 countries were recruited into the study in the 1990s, and at the time of enrolment all had a BMI <30 kg/m2 and were not considered to be obese. Researchers set out to assess the relationship between having asthma and becoming obese 10 years later. The study also analysed those who developed asthma over a 10-year period and their subsequent risk of becoming obese in the following 10 years.
Results showed that 10.2% of people with asthma at the start of the study period became obese 10 years later, compared to 7.7% of those who did not have asthma. Further analysis of the results revealed that the risk of obesity was even greater for those who developed asthma in adulthood, as well as in those who had asthma but who did not have allergies.
Until now there have been very few studies into whether asthma is a risk factor for obesity. Dr Subhabrata Moitra, ERS Research Fellow, ISGlobal, Barcelona Institute for Global Health, Barcelona, Spain, commented on the importance of the findings and where future research needs to be directed: “Our findings suggest the relationship between the two conditions is more complicated than we previously realised. It is important that we do more work to pick this apart. For example, we do not know why having asthma increases the risk of developing obesity or whether different asthma treatments have any effect on this risk.”
This research is an important step in helping clinicians and healthcare professionals to understand the relationship between obesity and asthma but also raises new questions regarding why the two are linked and what can be done to help patients, who are at the heart of all clinical research.
Treatment for Ureaplasma Infection May Reduce Respiratory Problems in Premature Babies
PREMATURE birth is related to a wide variety of health complications, not least for the respiratory system. Now, new research presented at the ERS Congress and reported in a ERS press release dated 14th September 2018 suggests that the presence of Ureaplasma in a premature baby’s windpipe is related to the development of serious respiratory disease. Not only that, data also show that treating this infection with a common antibiotic could be an effective option for combating this problem in the future.
“A key question is whether this bacteria is causing ill health in newborns and, if so, whether eliminating the bacteria improves outcomes for these very small babies,” explained Prof Rose Marie Viscardi, University of Maryland School of Medicine, Baltimore, Maryland, USA.
The study examined 121 premature babies born between 24 and 28 weeks’ gestation, all of whom were tested for the presence of Ureaplasma in their nose and windpipes; half of them were treated with the antibiotic azithromycin (20 mg/kg of subject weight/ per day), while the other half received placebo. Of the babies assessed, 36% were found to be Ureaplasma-positive, with the highest incidence being found in the most premature babies (45% of those born between 24 and 28 weeks).
The babies found to have the bacteria present in their windpipe were less likely to survive compared to those with the disease present only in their nose or those without the disease (71% versus 90% and 100%, respectively); they were also found to be more likely to develop bronchopulmonary dysplasia (67% versus 50% and 21%, respectively). Finally, the study showed that a 3-day course of treatment with azithromycin reduced the risk of death and severe respiratory disease 1 year after birth compared to placebo (33% versus 86%).
The authors were quick to caution that this study was limited by its small size and larger scale examination is needed before this antibiotic treatment can be more broadly adopted for these patients. Nonetheless, these results should encourage clinicians to look more closely at the impact of Ureaplasma infection in premature babies. “This study shows that Ureaplasma infection is very common in extremely premature infants and clinicians should consider testing for this infection in those newborns who are at risk,” concluded Prof Viscardi.
Macitentan: Safe and Effective for Portopulmonary Hypertension
PULMONARY VASCULAR RESISTANCE (PVR) in portopulmonary hypertension (PoPH) patients can be significantly improved with macitentan treatment, according to results of the PORTICO trial, which were reported in an Actelion Pharmaceuticals Ltd. press release dated 17th September 2018. Presented at the ERS Congress 2018, these results are consistent with those observed in previous trials and suggest a promising treatment option for PoPH patients.
Recognised as the fourth most common form of pulmonary arterial hypertension (PAH), PoPH is associated with cirrhosis and often only diagnosed during liver transplant assessment. In addition, data on PoPH therapies are limited and there are currently no PAH treatments that have been shown to improve cardiopulmonary haemodynamics of PoPH patients in randomised controlled trials.
To address this issue, researchers investigated the safety and efficacy of macitentan, an orally available endothelin receptor antagonist indicated for PoPH, in the first randomised controlled trial of its kind. The PORTICO trial was a placebo-controlled, double-blind study including 85 PoPH patients randomised 1:1 to receive placebo (n=42) or macitentan 10 mg (n=43) once daily during a 12-week period. After the treatment duration, the study’s primary endpoint of a reduction in PVR was achieved: the macitentan group showed an overall 35% reduction in PVR compared to placebo (geometric mean ratio: 0.65; 95% confidence interval: 0.59–0.72; p<0.0001). Additionally, macitentan significantly improved mean pulmonary arterial pressure by 5.99 mmHg (p<0.0001) and increased cardiac index by 0.52 L/min/m2 (p=0.0009) compared to placebo.
Macitentan was also well tolerated in the patient population, aligning with the known safety profile from previous trials, and the most commonly reported adverse events in ≥10% of the participants were peripheral oedema and headache. Since PoPH patients are commonly excluded from PAH clinical trials due to safety concerns, these are promising results for this patient population. In addition, lead investigator Prof Olivier Sitbon, University of Paris-Sud, Orsay, France, concluded: “The findings of PORTICO are relevant because if patients with PoPH can be treated to successfully lower pulmonary vascular pressure and resistance, more patients may be eligible for liver transplant as they will potentially have a better prognosis for this surgery.” Improvements in long-term quality of life for PoPH patients may, therefore, also be on the horizon.








