BACKGROUND
Regional pain syndromes are thought to be caused by soft tissue pathologies and are a frequent cause of musculoskeletal complaints. One of these syndromes, namely iliac crest pain syndrome (ICPS), is particularly common in patients with lower back pain (LBP). It is characterised clinically by pain perceived maximally at the most medial part of the posterior iliac crest. In addition, patients should recognise the pain provoked by a systematic digital palpation in this area as ‘their own’ typical pain.1 Though ICPS is very frequently encountered in LBP, the exact aetiology of this syndrome has not been established. Based on anatomical data, it was suggested that ICPS could be caused by a tendinopathy or enthesopathy of the erector spine (ES) muscle attachments to the medial iliac crest (MIC).2 In a previous anatomical and ultrasound (US) study we showed that this might be the case.3
AIMS
The purpose of this study was to test the ability of US and MRI to identify pathological transformations in the ES muscle entheses at the MIC in patients with LBP. Furthermore, we calculated the sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV), and the overall accuracy of the US and MRI to diagnose ICPS alongside clinical assessment to determine the gold standard diagnostic technique.
METHODS
A total of 25 patients (9 men and 16 women with a mean age of 43.12±11.83 and mean BMI of 25.07±2.36) with anamnesis of chronic, nonspecific (after lateral X-ray and standard clinical examination) LBP perceived maximally in the region of the MIC unilaterally or bilaterally were included in the study. First, a systematic palpation of the posterior MIC bilaterally was performed by an independent examiner to diagnose ICPS clinically. Then, over 2 successive days, each patient underwent MRI examination of the lower back (lumbar and sacroiliac regions), with an enlarged field of view in the sagittal plane, and a standardised US examination of the ES terminal tendons and entheses bilaterally (Figure 1).
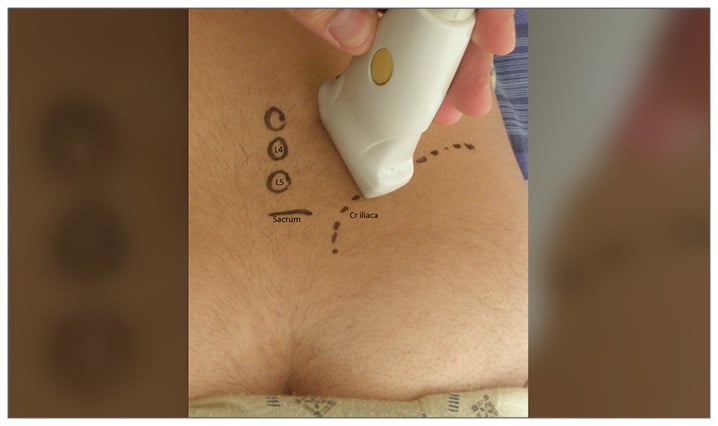
Figure 1: Position of the ultrasound probe for scanning of the right erector spine enthesis in the longitudinal plane (left side of the image is medial).
The MRI data were assessed by a radiologist with 10 years of MRI experience. The sonographies were performed and analysed by a rheumatologist with 7 years of US experience and analysed in accordance with the OMERACT definition of enthesopathy.4 Both the radiologist and the sonographer were blinded to the clinical findings of the given patient.
RESULTS
Clinical examination (palpation) identified 25 painful ES entheses of the total 50 cases examined, while MRI revealed pathology in 21 of the 50 ES entheses and US showed 27 of the 50 pathological ES entheses.
Based on these findings, the sensitivity, specificity, PPV, NPV, and overall accuracy of the US and the MRI for the assessment of ES entheses were calculated (at structure; i.e., an enthesis level) (Table 1).
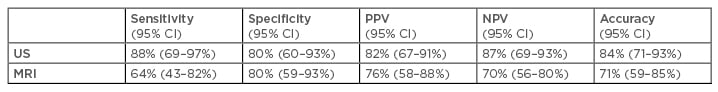
Table 1: Summary of the tests performed to compare ultrasound and MRI for the diagnosis of erector spine muscle entheses in patients with lower back pain.
CI: confidence interval; NPV: negative predictive values; PPV: positive predictive values; US: ultrasound.
CONCLUSION
This study shows that both US and MRI have good capability to identify pathological transformation in the ES entheses in patients with nonspecific LBP. US and MRI showed equal specificity but US had greater sensitivity. These diagnostic properties of US could be of value when assessing patients with otherwise nonspecific LBP, especially those likely to have soft tissue regional pain syndromes like ICPS.
DISCUSSION RAISED
Discussion at the presentation was about the fact that soft tissue rheumatic pain is frequently overlooked in patients with LBP, despite it being very common. It was also mentioned that a clinician should maintain their anatomy knowledge to be a good diagnostician. Finally, it was emphasised that this study opens the door for a new diagnostic application of musculoskeletal US, namely in patients with LBP of clinically unidentified origin.








