Ankylosing spondylitis (AS), a chronic inflammatory rheumatic disease characterised by inflammation of the sacroiliac joints and the spine,1 has a reported prevalence between 0.2% and 0.5% in the USA.2 However, the true prevalence of AS is unknown due to significant diagnosis delays and under-recognition of disease. A study based in the USA3 demonstrated that patients with AS experience a significant delay (on average 14 years) from AS symptom onset to diagnosis. Understanding the diagnostic journey of patients with AS and identifying opportunities to quickly diagnose and appropriately refer patients is therefore critical to reducing time to diagnosis, preventing irreversible joint damage, and preserving mobility. This study aimed to describe the patient journey to AS diagnosis from the patient’s perspective and identify sex differences via a web-based survey.
Adults from the USA aged ≥18 years with a self-reported diagnosis of AS were recruited through outreach on social media and using CreakyJoints, an online patient support community comprising patients with arthritis and arthritis-related diseases and their caregivers. Survey questions were developed following analysis of qualitative interviews of patients with AS and clinical experts, as well as a targeted literature review. Respondents completed a web-based survey on sociodemographics, clinical characteristics, diagnosis history, and impact of AS on work and relationships. Survey results were compared between women and men using the 2-sample T-test for continuous variables and a chi-squared test for categorical variables.
Among 235 respondents, 174 (74.0%) were women. On average, men were older than women (mean: 53.1 years [standard deviation (SD): 10.3] versus mean: 48.6 years [SD: 10.6], respectively); however, women had worse disease severity. Overall, the mean time from symptom onset across all respondents was 17.9 years (SD: 12.6) and the mean time since official diagnosis was 8.5 years (SD: 9.3). The most common symptoms that led to seeking medical care were back pain, joint pain, stiffness, and fatigue (Figure 1A). Women were more likely than men to seek medical care due to foot problems (31.6% versus 11.5%, respectively), whereas men were more likely to seek care due to uveitis (31.1% versus 14.9%, respectively; both p<0.05). During diagnosis, respondents most commonly reported seeking medical care from a general practitioner (87.2%) and rheumatologist (65.1%), with no differences between women and men. The most commonly reported misdiagnoses were back problems (55.7%), psychosomatic issues (23.0%), and sciatica (21.3%) in men, whereas psychosomatic issues (40.8%), back problems (40.2%), and anxiety and depression (23.6%) were most common in women. Significantly higher proportions of women than men reported misdiagnoses of psychosomatic issues (40.8% versus 23.0%, respectively) and fibromyalgia (20.7% versus 6.6%, respectively) (Figure 1B). All respondents reported a significant impact of their AS on work and relationships, with women more likely to report an impact on aspects of their relationships than men.
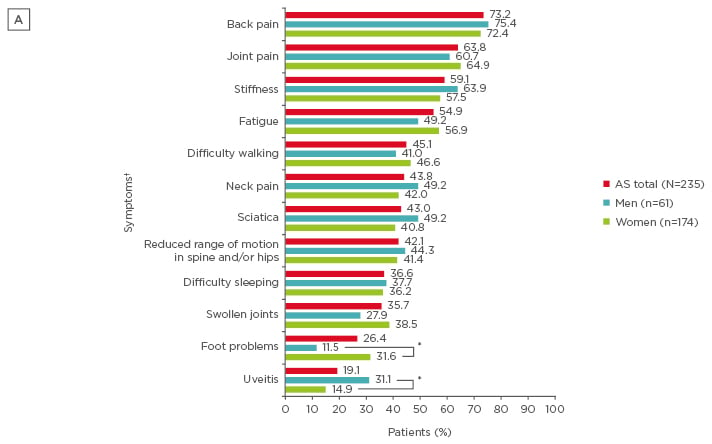
Figure 1A: The most common first symptoms in patients with ankylosing spondylitis to prompt seeking medical care.
*p<0.05 for comparisons between men and women; † Respondents were able to select >1 option.
AS: ankylosing spondylitis.
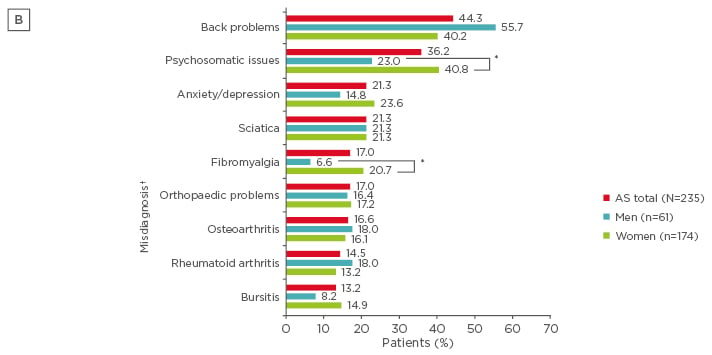
Figure 1B: The most common misdiagnoses in patients with ankylosing spondylitis.
*p<0.05 for comparisons between men and women; † Respondents were able to select >1 option.
AS: ankylosing spondylitis.
These survey findings highlight differences between men and women in initial symptom presentation, misdiagnoses, time to diagnosis of AS, and impact of AS on work and relationships. Early recognition of symptoms associated with AS and understanding potential sex differences in symptom presentation over time will help reduce misdiagnoses and shorten the time to diagnosis of AS, leading to improved care and health-related quality of life.








