Abstract
Knee infection is a challenging scenario. One way to classify the infection would be as spontaneous or post-surgery, the latter having a particular relevance given the presence of synthetic materials such as screws or prostheses surrounding the joint. Open surgery has a higher rate of infection than arthroscopic procedures. Periprosthetic infection is a complication that follows arthroplasty, with an incidence that varies between 0.4% and 2.0%, while arthroscopic procedures have an incidence varying between 0.001% and 1.100%. Anterior cruciate ligament (ACL) reconstruction complication rate is low, with septic arthritis one of the most frequently seen. Early diagnosis of complications is vital to improve functional outcome. In these cases, knee pain, decreased range of motion, fever, and high C-reactive protein levels should alert any physician, and infection must not be ruled out. This article presents a case of infection after ACL reconstruction and discusses risk factors, treatment choice, antibiotic treatment length, and functional outcomes, proposing a guide for the treatment. The clinical case presented is a chronic infection due to Staphylococcus aureus that resulted in extensive cartilage damage and graft loosening; delayed diagnosis was an essential modifiable risk factor in this case. Treatment success is defined as the eradication of the infection without the need to remove the ACL graft. Risk factors for a worse outcome after ACL reconstruction infection are allograft compared to autograft and S. aureus or polymicrobial infection compared to coagulase-negative staphylococcus infection. Functional outcome is compromised by infection; however, if early diagnosis and treatment are performed, good functional results and a return to sports activities can be expected.
INTRODUCTION
Acute septic arthritis is a common clinical problem seen in emergency departments, and the knee is the most frequently affected joint. Despite advances in medicine, septic arthritis is still a significant cause of morbidity and sequelae.1 Knee infection can be classified as spontaneous or post-surgery, with the latter commonly due to the presence of osteosynthesis or prosthesis material. Open surgery has a higher rate of infection than arthroscopic procedures. Periprosthetic infection is a complication that follows arthroplasty and the incidence varies between 0.4% and 2.0%, while arthroscopic procedures have an incidence that varies between 0.001% and 1.100%.2,3
The anterior cruciate ligament (ACL) is an intra-articular and intrasynovial structure of the knee, which plays a crucial role in joint stability.4 ACL tear incidence is increasing; the most frequent mechanism of ACL tear is an indirect, involuntary torsion known as pivot shift, which consists of a valgus and internal force applied to a knee at a flexion degree of 10–20°.5 General consensus is that anatomical ACL reconstruction can restore anteroposterior and rotatory stability,6 but graft choice depends on different factors, with the most important being the surgeon’s preference and patient’s preference, patient activity, and history of prior surgery.7 The most commonly used grafts are bone-patellar tendon, hamstrings (HT), bone-quadricipital tendon, and allograft.8 Although rare, ACL reconstruction has complications. Cvetanovich et al.9 reviewed the complications of ACL reconstruction in the first 30 days and found the major complication rate to be 0.55%, with deep vein thrombosis the most frequent; pulmonary embolism and infection were also observed.9 Other studies report similar complication rates and show that infection is one of the most frequent complications after ACL reconstruction, with an incidence between 0.14% and 1.70%.10-13
This article presents a case of infection after ACL reconstruction and discusses the risk factors for infection, treatment choice, antibiotic treatment length, risk factors for treatment success, and functional outcomes, concluding with a guide for treatment.
CASE REPORT
A 40-year-old male was evaluated in the emergency department complaining of 2 weeks of intermittent fever, quantified up to 38.5°C, and left knee pain associated with articular effusion and a loss of range of motion. His clinical record showed a left knee ACL reconstruction with bone-patellar tendon-bone (BTB) graft 4 months prior to emergency department admission. After surgery, he did not recover normal articular range and had intermittent severe pain. Two months after surgery, he was diagnosed with articular stiffness and an arthroscopic fibrous tissue debridement, and mobilisation under anaesthesia were performed. No cultures were taken on this occasion. Both procedures were performed in other institutions.
RISK FACTORS
Many variables have been studied to determine if they are a risk factor for infection after ACL reconstruction. In a recent meta-analysis performed by Murphy et al.,14 a multivariate logistic regression was estimated in a cohort of 1,397 ACL reconstruction patients for risk factors for infection. Significant factors noted were age >20 years, male sex, connective tissue disease, consumption of immune suppressive medications, and HT graft. Diabetes and previous ipsilateral knee surgery were not statistically significant variables.14 Despite this finding, a study by the MOON Knee Group showed a higher incidence of infection in diabetic patients following ACL reconstruction.15 Krutsch et al.16 compared infection rate by sport and found that football had a higher rate of infection than skiing, suggesting that ambient temperature must affect infection rates.16 In addition, Westermann et al.17 performed a multivariate analysis in a cohort of 6,389 ACL reconstruction patients comparing infection rates between outpatients and hospital-admitted patients. The authors found a significant increase in the rate of infection in admitted patients and concluded that efforts must be made to improve outpatient care.17
A recent meta-analysis performed by Bansal et al.18 showed a lower infection rate when a BTB graft was used compared to HT autograft, reaching a relative risk of 0.230 (95% confidence interval: 0.097–0.540) and a heterogeneity of 0%. This meta-analysis did not find a significant difference in infection rates for autograft versus allograft, achieving a relative risk of 1.035 (95% confidence interval: 0.589–1.819) and a heterogeneity of 0%.18 Likewise, another recent cohort study of 10,190 ACL reconstructions performed with allograft showed an infection rate of 0.15%, highlighting that the newest evidence shows no increased risk of infection if an allograft is used.19
Graft contamination is a risk for the development of septic arthritis.20,21 Accidental contamination of the graft is a modifiable risk factor and is important to consider in graft contamination prevention. If this happens, there are protocols for treating the contaminated graft, which include the use of gentamicin and chlorhexidine, obtaining negative cultures of >90%.22 The current consensus in cases of contamination, regardless of the type of autograft (BTB or HT), is to perform a washing procedure with saline solution and an antibiotic or disinfectant for 8 minutes. The recommended method is to use gentamicin or 2% chlorhexidine, achieving negative cultures of approximately 100%. There are no established guidelines for allografts.12,23,24
In addition to accidental contamination, such as incidence of the graft falling to the ground, there is concern about the contamination of the graft as it was placed on the surgical table. Alomar et al.25 performed a case-control study in which they took cultures of a dropped graft (case) and a graft that was always kept on the surgical table (control). The dropped graft showed a trend towards more positive cultures; nevertheless, no significant difference was achieved. In both groups, Staphylococcus epidermidis was the most commonly found bacteria, followed by S. aureus in the control group and by Bacillus species in the case group. Notably, the control group showed epidemiology more likely to be an ACL reconstruction infection than the control group.25
In the authors’ own experiences, after preparation, the graft is kept in a glass container, submerged in a saline solution with 80 mg of gentamicin; this is maintained until it is time to start the fixation, and the process does not alter the biomechanics of the graft. Also, all patients receive 2 g of cefazolin before surgery and two doses of 2 g cephazolin after the surgery. Referring to the aforementioned case study, except for age (40 years), the patient did not present other risk factors for infection. It is noteworthy that there was no history of what happened to the patient between the two previous surgeries, such as accidental contamination of the graft, for example.
DIAGNOSIS
The most common symptoms of infection following ACL reconstruction are fever, knee effusion, loss of knee flexion, and pain.26 According to Wang et al.,27 the median number of days after surgery for symptom presentation is 13. It is important to emphasise the transcendental nature of early diagnosis since it increases the possibility of retaining the graft and avoids severe cartilage damage and ankylosis.28,29
Laboratory tests are essential to confirm the diagnosis. In a study by Wang et al.,30 comparisons between C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) in noninfected and infected ACL reconstruction patients at 5 days post-surgery demonstrated that a CRP >41 mg/dL had a sensitivity of 94.1% and a specificity of 97.6%, while ESR >32 mm/hour had a sensitivity of 91.2% and a specificity of 80.5%.30
Infections are classified by time after surgery as acute (<3 weeks after surgery), subacute (3 weeks to 3 months after surgery), and chronic (>3 months after surgery), with acute and subacute the most common. The most frequent infection-causing agents were the Staphylococci, with the most common, S. epidermis, responsible for 50% of incidences (coagulase-negative staphylococcus [CNS]), followed by S. aureus. Fungus infections by Candida and Aspergillus have also been reported and are associated with high rates of graft removal and worse functional outcomes compared to Staphylococcus infection.31 Also, tubercular infection cases have been reported, so endemic zones must include this infection in diagnosis algorithms.32
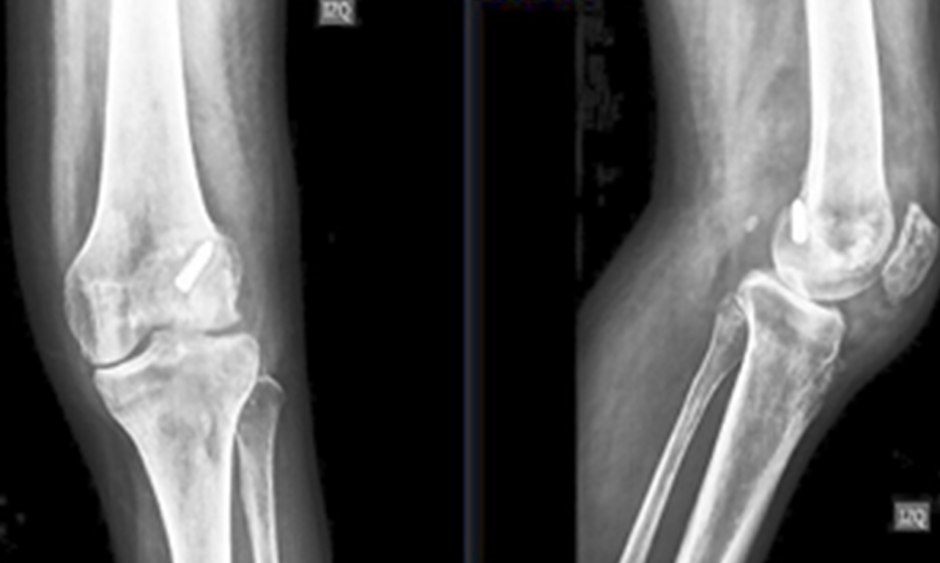
In the reported case, physical examination showed an axillary temperature of 37.8°C, a significant increase in local temperature, 10° of passive articular range of motion (-20° extension and 30° flexion), and a moderate amount of effusion. This was recognised as a classic presentation of joint infection and it was probably a chronic presentation due to the time elapsed since surgery and beginning of the symptoms. Knee X-rays and laboratory tests were performed; the X-rays showed osteolysis around the femoral metallic screw and loss of the definition of the distal edge of femur, especially in the lateral condyle (Figure 1), confirming that the infection was not acute. The CRP and ESR values were 175 mg/L and 50 mm/hour, respectively, values that are above the cut-off values described by Wang et al.30

Figure 1: X-rays of the damaged knee joint taken at the emergency department.
Osteolysis around the femoral screw and loss of the definition of the articular edge of the femur, more significant in the lateral condyle, were the most notable findings.
TREATMENT
Arthroscopic irrigation and debridement, graft retain, and antibiotic therapy are the treatments of choice, reaching a success rate of 85%.33 Graft debridement is only encouraged if a loss of tension is found during arthroscopy procedure, if purulent exudation has adhered to the graft, or in cases of persistent infection after 2–3 arthroscopic irrigation and debridement.34 Treatment must be monitored clinically and using laboratory examinations. A 50% decrease in CRP value must be expected after 48 hours of treatment and normal values must be reached between 10 and 14 days.30
Some authors suggest no surgical treatment. Viola et al.35 proposed only antibiotics; meanwhile, Monaco et al.36 proposed antibiotics and joint irrigation. These authors report a rate of change to the surgical treatment of 42.9% and 30.0%, respectively.35-36 A literature review by Wang et al.37 showed that 153 out of 176 (86.9%) patients with infection underwent surgery, and 39.8% of them required more than one surgical procedure. The need for a second surgical procedure depends on the evolution of symptoms; if fever, knee effusion, or decreased range of motion persist or laboratory exam results do not improve within 48–72 hours of treatment, the patient must undergo another surgical procedure.38,39 When the decision to perform graft debridement is made, all screws or other devices must be removed because keeping sutures or such devices can maintain symptoms even after graft removal.39
The duration of intravenous (IV) antibiotic administration and the total length of antibiotic treatment are topics of debate. Some authors recommend IV antibiotics for 14–21 days; another recommendation is to use antibiotics until the CRP value reaches ≤50 mg/dL and no fever is present, which normally occurs after 5–7 days. On the other hand, Pérez-Prieto et al.40 proposed an oral treatment with levofloxacin and rifampicin as soon as cultures are available, a treatment which should be continued for 6–8 weeks, with no more than 3–4 days of IV treatment. In their report, Pérez-Prieto et al. only included acute cases, and reported a normalised ESR and CRP after 3 weeks of oral treatment plus surgery. Their graft removal rate was 1 of 15 patients (0.6%).40
Since the evidence available is only from consensus and case series, we should be very critical of the available information in the literature. The data show a trend that patients who are treated with longer periods of IV antibiotics are associated with surgical irrigation and debridement, have a shorter duration of symptoms, and experience an early decrease in CRP and ESR.13,17,34,37
The authors of this review recommend surgery as soon as possible after diagnosis is made, starting empirical treatment once the cultures are taken. The authors use cephalosporin as empirical treatment and adjust by culture results and antibiogram. If the symptoms persist or the inflammatory parameters remain stagnant using the correct antibiotic according to antibiogram, a second surgical procedure is performed as soon as possible. In the case presented, the authors were even more prompt with the indication of the second procedure, given that it was a chronic presentation that caused much joint damage and had extensive fibrotic tissue. Regarding antibiotic treatment, the authors’ policy is to maintain IV antibiotic treatment until CRP reach normal values (<20 mg/dL), which normally occurs between Day 10 and 14; following this, oral antibiotics are administered until 6 weeks of treatment have been completed.
In the case presented, arthroscopic irrigation and debridement was performed at 3 hours after admission. Arthroscopy showed extensive compartmentalisation of the knee due to fibrous tissue and a rotten and loose graft. Also, the femoral screw was completely loose and was easily removed with a grasper without any help of a screwdriver. In the medial and lateral compartment, an important loss of meniscal tissue and extensive and diffuse Grade 3 International Cartilage Research Society (ICRS) classification chondral damage in both condyles and tibial plateaus was observed (Figure 2). Irrigation was completed with 24 L of saline solution and debridement of fibrous tissue with a shaver was performed. Four tissue samples were cultured, as well as a sample of articular liquid and the metal screw of the femur. After taking cultures, 2 g of cefazolin every 8 hours was started.
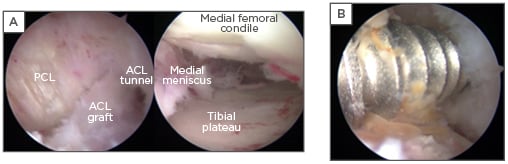
Figure 2: Arthroscopic images obtained during irrigation and debridement.
A) After debridement of an extensive anterior fibrous tissue, the ACL graft was identified. The graft was completely loose, the femoral tunnel was widened, and the screw was removed with a grasper clamp, without the help of a screwdriver, and purulent exudate surrounded it. B) The medial compartment. Extensive cartilage and meniscus damage was observed in both the lateral and medial compartments.
ACL: anterior cruciate ligament; PCL: posterior cruciate ligament.
Treatment success is defined as the eradication of the infection without the need to remove the ACL graft. Various factors have been studied to predict the success of treatment. When arthroscopic irrigation and debridement and antibiotics are used for treatment, no difference in treatment success exists between autografts (bone-patellar tendon, CT, or HT). Meanwhile, allograft has a higher failure rate compared to autograft. Another risk factor for treatment failure is S. aureus or polymicrobial infection compared to CNS infection. As noted, fungal infections have a high risk of sequelae;31 on the other hand, negative cultures are a protective factor.33
The patient reported in this case had many factors of a bad prognosis: infection with S. aureus, chronic presentation, and substantial joint damage, so immediately the graft and screws were removed. After 2 days of treatment, the patient recovered 50° of knee range of motion (-20° extension and 70° flexion), and his pain decreased considerably. However, the local temperature still increased, and inflammatory parameters remained unchanged (Figure 3). As a consequence, a second arthroscopy irrigation and debridement was performed. Irrigation with 18 L of saline solution was conducted, and two perforations with a 4.5 mm drill were performed in the tibia, guided with a tibial compass in 60° to decompress the tibial tunnel.
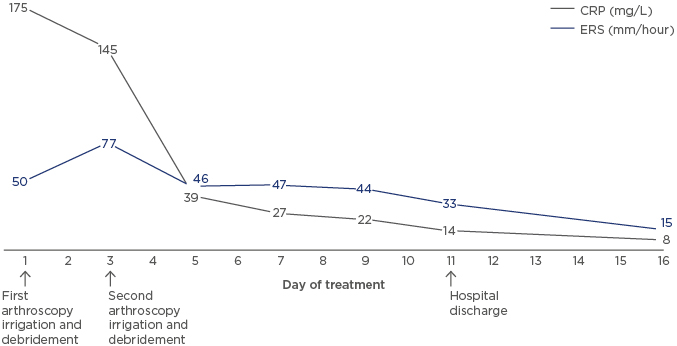
Figure 3: C-reactive protein (mg/L) and erythrocyte sedimentation rate (mm/hour) behaviour from Day 1–16 of treatment.
On Day 1, the first arthroscopy irrigation and debridement was performed. On Day 3, after CRP and ERS results, the second arthroscopy irrigation and debridement was performed. Hospital discharge was on Day 11.
CRP: C-reactive protein; ESR: erythrocyte sedimentation rate.
FUNCTIONAL OUTCOMES
Return to any sporting activities after ACL reconstruction occurs in 80% of cases and return to the same level of activity is experienced by 65% of patients.41 Makhni et al.,22 in a recent meta-analysis, reported a 67% return to sports, 13% knee instability, and a median score of 82.1 in the Lysholm Knee Scoring System after infection following ACL reconstruction.22 Windhamre et al.,38 in a recent study, demonstrated that all patients achieved an improvement over their functional score before reconstruction; however, they tended to have lower functional outcomes to similar groups that were not infected.38
In cases of graft removal, ACL revision, in which a new reconstruction of the ACL occurs, is a treatment option. Most authors recommend revision after 6–12 months.13,37 Hantes et al.34 published a case series of ACL revision after infection with excellent functional outcomes with a follow-up of 6.3 years (4–9 years). They performed revision with an ipsilateral BTB autograft after 5–9 months of treatment in 4 of 6 patients. They achieved a Lysholm Knee Scoring System score of 92 (87–95) and a difference of anterior translation of the tibia between the two knees of the patient of 1.4 mm (measured by the KT-1000 test).34
The medical literature regarding post-infection ACL revision is limited to case reports. The authors of this report follow an algorithm similar to prosthetic infection scenario, in which it is requisite that the infection is controlled for the following surgical procedure, in this case, ACL revision. The minimum required to establish control of the infection is to maintain CRP and ESR at normal values after 1 month of having completed the antibiotic treatment, and, at any minimum suspicion of infection, an arthrocentesis for synovial fluid cultures must be performed.42 The procedure itself must be addressed and planned like any ACL revision. The decision to perform revision as either a one or two-step procedure time depends on the size of the tunnels (femoral and tibial). Two-step revision firstly requires the filling of the tunnels with a bone graft, then waiting 4–6 months for graft incorporation, and in the second procedure, ACL reconstruction is carried out.43
After the second arthroscopy irrigation and debridement, the patient’s condition improved, achieving a joint range of -10° extension and 80° flexion, and considerably less pain. After 10 days of IV treatment, the patient achieved a normal CRP of 18 mg/L and was discharged with cefadroxil 1 g every 12 hours until 6 weeks of treatment were complete. One week after discharge, the patient had significantly less articular effusion, a functional knee range of motion (-5°/90°), and was walking with partial weight bear and two canes. His inflammatory parameters continued to decrease (CPR 8 mg/L and ESR 17 mm/hour) (Figure 3). Six months after surgery, the patient resumed his work activities (desk work), had no complaints of instability in daily life activities, had normal CPR and ESR levels, and had a full range of motion. For now, there are no plans to carry out an ACL revision on this patient.
CONCLUSION AND RECOMMENDATIONS
Delayed diagnosis of infection after ACL reconstruction is catastrophic, compromising functional outcome and cartilage survival, as documented in the case reported in this article. Therefore, the authors recommend a prompt and comprehensive diagnosis before any suspicion of infection. Early treatment improves the functional result and is very important to preserve the graft. The gold standard treatment is arthroscopic irrigation and debridement with graft retaining and antibiotics, achieving 85% success. On the other hand, in cases like the one reported in this review, in which factors of bad prognosis are present, the authors recommend removal of synthetic material, such as a screw, and graft removal. Among the risk factors for infection reported in the literature, the most consistent is the use of HT graft. Other reported risk factors are age >20 years, diabetes, and the use of immunosuppressive drugs.
The most common agents of infection are Staphylococci; as a result, cephalosporin or vancomycin should be used as initial IV treatment until cultures are available. The duration of IV antibiotic administration and total length of antibiotic treatment are topics of debate, and the authors strongly recommend that antibiotics are used until the CRP is <20 mg/dL. Infection compromises functional outcome; however, if treatment is started early, good functional results and a return to sports activities can be achieved. If the graft must be removed, ACL revision requires no signs of infection for at least 1 month after having completed antibiotic treatment.