Abstract
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease that involves collagen tissue throughout the body. Several previous studies have shown that the risk of ischaemic and haemorrhagic stroke is significantly higher in SLE when compared to the general population, particularly in young individuals, representing one of the principal causes of death in these patients. Though the precise pathophysiology behind this increased risk is still poorly understood, several mechanisms are suggested to play a role. The high burden of cerebral small vessel disease features noted on brain neuroimaging studies, as well as the accelerated process of atherosclerosis identified in these patients, are likely to be responsible for at least some of the ischaemic strokes occurring in the SLE population. Repeated episodes of arterial and venous thrombosis secondary to antiphospholipid syndrome are likewise important. Less is known regarding the exact pathophysiological relationship between SLE and the high incidence of haemorrhagic stroke, though thrombocytopenia and a greater susceptibility to form typical and atypical brain aneurysms, which may then rupture, are thought to be the main mechanisms responsible for the occurrence of intracerebral and subarachnoid haemorrhage, respectively. Both inflammatory and noninflammatory events, all involving the immune system, are responsible for several pathological changes affecting cerebral vessels of every calibre in SLE, as confirmed by histopathology. In this context, endothelial activation and dysfunction play a critical role. This review will briefly analyse the most important factors responsible for the higher ischaemic and haemorrhagic stroke risk in the SLE population, with a particular focus on brain vascular changes.
INTRODUCTION
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder that causes inflammation in connective tissues throughout the body. Prevalence ranges from a few to 241 cases per 100,000 people, with women and people of black ethnicity being more frequently affected.1 Numerous studies have shown that individuals with SLE have a higher risk of cerebrovascular events than the general population.2,3 Stroke and cerebrovascular events in general are among the main specific causes of death in SLE patients, representing 10–15% of all deaths in this population.4
It has been demonstrated that in patients with SLE, the risk of any kind of stroke, ischaemic or haemorrhagic, is higher when compared to the general population, particularly in patients <50 years old.2,5,6 Specifically, studies have reported a 2-fold increased risk for ischaemic stroke and 2–3-times greater risk for intracerebral haemorrhage (IH) in SLE patients in comparison with the general population.2,5 Moreover, apart from overt neurological syndromes, silent vascular damage, evaluated with MRI, is augmented in SLE.5 Subarachnoid haemorrhage (SAH) also seems more frequent in SLE patients compared to the general population, with a reported incidence rate of 49.4 versus 10.2 per 100,000 person-years.7 Although the exact mechanisms responsible for the increased stroke risk in SLE are not yet fully understood, numerous hypotheses have been formulated. The aim of this review is to analyse the different factors contributing to the higher risk of stroke in the SLE population, with a focus on cerebral vascular changes (Box 1).
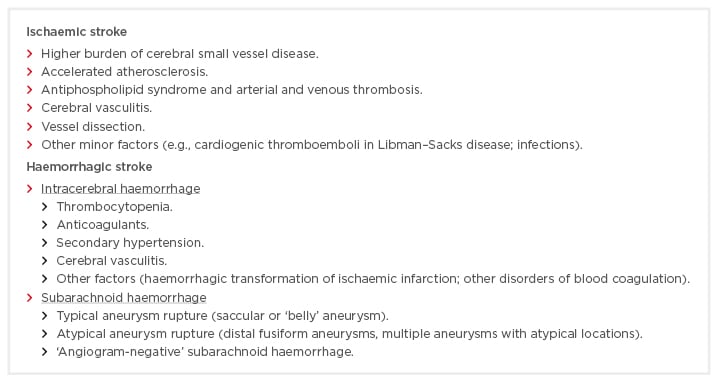
Box 1: Principal factors implicated in the higher stroke incidence in systemic lupus erythematosus patients.
CEREBRAL VASCULAR CHANGES IN SYSTEMIC LUPUS ERYTHEMATOSUS AND THE ROLE OF ENDOTHELIUM
It is widely known that vascular involvement in SLE is a key factor for the development of numerous central nervous system pathological manifestations.8 Both inflammatory and noninflammatory events affect cerebral vessels of every calibre. As further described below, all cerebral vessels, from large arteries to small vessels to veins, can potentially be involved in SLE.
Such a diffused vascular participation has been confirmed by numerous pathological studies reporting several changes affecting brain vessels, ranging from thrombosis, perivascular infiltration of inflammatory cells, and destructive and proliferative changes, comprising fibrinoid degeneration and endothelial cell proliferation.9,10
All of these mechanisms involve the immune system with different events: immune complex/complement injury, vasculopathy due to antiphospholipid (aPL) antibodies or dysfunctional platelets, plasma factors, endothelial cell adhesion molecules, and overt clotting due to aPL antibodies resulting in thrombosis or cardiac emboli to the brain.11
It would appear that the key factor in the pathogenesis of all of these events is endothelial cell damage and/or activation.8,12,13 It is known that one of the main mechanisms involved is the direct binding of autoantibodies to certain molecules expressed on the surface of endothelial cells, such as beta 2 glycoprotein I, which is considered to be among the most important.12 This process, together with immune complex depositions, increases complement-dependent cytotoxicity and endothelial permeability and leads endothelial cells to express adhesion molecules, which attract circulating lymphocytes and monocytes. Atehortúa et al.14 have also hypothesised a possible interaction of different monocyte subpopulations with endothelial cells, favouring alterations in the macro and microvascular context of SLE. The combination of these processes leads to prothrombotic activity induction, leukocyte subendothelial infiltration, and detachment of endothelial cells; for example, an increased number of circulating endothelial cells have been found in the blood of patients with SLE.15 A peculiar susceptibility of the brain endothelium to these inflammatory mediators in comparison with endothelial cells from other anatomical regions has also been hypothesised.12
ISCHAEMIC STROKE
Cerebral Small Vessel Disease
One of the hypotheses for the higher stroke incidence in SLE patients is related to the association between SLE and cerebral small vessel disease (CSVD).
The term CSVD refers to various pathological processes affecting the perforating cerebral arterioles, capillaries, and venules of the brain, with subsequent parenchymal damage, mainly in the white matter and in the subcortical grey matter.16 CSVD is very common, accounts for approximately 20% of all strokes, and increases the risk of future strokes by >50%;17 symptoms include cognitive and balance impairment and dementia. Neuroimaging, particularly MRI, is essential for the diagnosis of CSVD, and some scores based on MRI features, such as lacunes, white matter hyperintensities, cerebral microbleeds, and enlarged perivascular spaces, have been developed to calculate a total CSVD burden, thus providing a standardised language and a baseline stratification of patients with CSVD.18 Using MRI features, Wiseman et al.19 showed that patients with SLE have a high burden of CSVD; MRI-dependent CSVD score was higher in SLE patients when compared to both healthy control patients and patients with minor stroke, despite the latter presenting more traditional cardiovascular risk factors.
Although the correlation between SLE and CSVD is not yet fully understood, it is hypothesised that inflammation, as it is the underlying factor in SLE, might well play an important role in the pathogenesis of CSVD. Pathological studies have showed inflammatory infiltrates in the perforating arteriolar walls,20 and some authors have reported an association between the levels of C-reactive protein (CRP) and CSVD-related lesions.21 Moreover, enlarged perivascular spaces, the MRI feature mainly responsible for the higher CSVD score in SLE patients,19 have been shown to be associated with increased plasma markers of inflammation,22 as well as with other inflammatory brain disorders such as multiple sclerosis.23 Therefore, it is likely that some endothelial damage risk factors occurring in SLE, such as complement activation and immune complex deposition, could stimulate cerebrovascular inflammation, causing a high burden of CSVD, and are responsible for at least some of the ischaemic strokes in SLE patients.19
Accelerated Atherosclerosis
Numerous studies have identified an accelerated, premature process of atherosclerosis as one of the leading causes of the elevated risk of ischaemic stroke and cardiovascular events in patients with SLE.24-28 Various hypotheses have been formulated to explain this phenomenon. Firstly, an increased prevalence of several traditional risk factors for atherosclerosis have been shown in the SLE population. Hypertension in particular has been found to be the most important traditional factor associated with SLE.27 Diabetes also seems to be more common in SLE patients than the general population.6,26 Furthermore, these patients are more likely to have a more sedentary lifestyle, higher very low-density lipoprotein-cholesterol and triglycerides, and lower high-density lipoprotein.24,26
However, traditional risk factors alone fail to explain the excess risk of atherosclerosis in SLE patients,29 especially when the trend for higher stroke risk in people <50 years old is considered. A further confirmation also comes from some studies that found SLE to be associated with a high burden of early atherosclerosis even after adjustment for classic risk factors was made.28,30 Therefore, other SLE-related factors must be considered to explain the high atherosclerotic burden in these patients. Once again, systemic inflammation seems to play a pivotal role in the atherogenic process. It is known that inflammation is involved in all stages of atherogenesis, from the formation and evolution of atheroma to the thrombotic complications of this disease.31 CRP has been demonstrated to be an active mediator in the pathogenesis of atherosclerosis,31 and elevated levels of CRP have been found during the course of SLE, even in patients with inactive disease,27 thus representing another factor involved in the accelerated atherosclerosis in SLE. SLE-related inflammation also contributes to several dyslipidaemic alterations associated with the development of atherosclerotic disease, such as hypercholesterolaemia, hypertriglyceridaemia, and the reduction in activity of lipoprotein lipase and other antioxidant enzymes.26
Autoimmune phenomena also play an important role in the atherogenic process. SLE-circulating immune complexes have been shown to stimulate the accumulation of cholesterol in cultured smooth muscle cells.32 SLE autoantibodies, such as double strand-DNA autoantibodies and, when present, aPL antibodies, stimulate endothelial activation, which is considered one of the main and earliest steps in the atherogenic process. Enhanced endothelial activation is also demonstrated by the increased serum levels of some markers, such as vascular cell adhesion molecule-1 (VCAM-1), thrombomodulin, and von Willebrand factor, which have been shown to be augmented in SLE patients, even with inactive disease.27
Another important element in the development of atherosclerosis in the SLE population is an altered vascular remodelling, as proven by the elevated levels of some metalloproteinases, like MMP-3, found in the serum of these patients, and this increased activity has been demonstrated during many steps of atherosclerosis.27,33 Several studies have shown that disease duration and damage index are also directly related to atherosclerosis.25,28,29
Conversely, the role of treatment, especially steroids, has not yet been fully established. Most authors have reported a direct correlation between elevated exposure to corticosteroids and the process of atherosclerosis.26,34 Roman et al.,28 on the other hand, found that SLE patients with carotid plaque presented lower average dose of prednisone than SLE patients without plaque. Antimalarials, in contrast, have generally been considered to have a beneficial anti-inflammatory and antiplatelet effect and have been associated with lower total cholesterol and triglyceride levels.26,35 Other nontraditional factors, such as chronic renal impairment and homocysteine levels, have also been related to the accelerated atherogenesis occurring in SLE.24,27
Antiphospholipid Syndrome and Thrombosis
It has been noted that 25–40% of SLE patients have secondary aPL syndrome (APS), characterised by the presence of aPL antibodies with clinical features of repeated episodes of arterial or venous thrombosis, recurrent spontaneous abortions, or thrombocytopenia.36 APS is a disorder characterised by thrombosis, which can be either venous, arterial, or both, and pregnancy loss in conjunction with the presence of lupus anticoagulant, or IgG or IgM anticardiolipin, or IgG or IgM anti-β2-glycoprotein I.37 The syndrome can be primary, when it occurs in the absence of any other related disease, or secondary, when it is associated with other autoimmune diseases, especially SLE (APS/SLE).36
In 2014, Kaichi et al.38 retrospectively examined 256 SLE patients (45 with APS, 211 without APS) who had undergone MRI studies. They found a higher incidence of cerebral lesions in patients with APS/SLE. Large territorial infarctions, lacunar infarctions in the deep white matter, localised cortical infarctions in the middle cerebral artery (MCA) territory, bilateral border zone infarctions, anterior basal ganglia, and stenotic arterial lesions were found to be more common in SLE patients with APS than in those without.38 The main factor responsible for vascular damage in APS/SLE is thought to be arterial and/or venous thrombosis. Arterial damage could be divided into large-artery occlusions (most commonly MCA) or into multifocal arterial stenoses. Focal regions of arterial narrowing have been noted within branches of the anterior, middle, and posterior cerebral arteries.39
Venous occlusive disease has also been described in the intracranial circulation;40 occlusion of dural venous sinuses and deep cerebral veins was reported with a prevalence of 29% in patients with APS.41
aPL antibodies are a heterogeneous family of antibodies that react against several anionic phospholipid-binding plasma proteins.12 The presence of this family of autoantibodies in the serum, operating through cofactors (β2-glycoprotein I or prothrombin), can generate a thrombotic diathesis. Although the mechanism for this hypercoagulable state is not yet fully understood, it appears to involve interactions between the antibodies to anionic phospholipid-protein complex and antigen targets on platelets, endothelial cells, or components of the coagulation cascade.42
Therefore, APS is likely to represent a key factor in the origin of ischaemic and venous stroke in SLE patients, as also reported by Valdés-Ferrer et al.,43 who described a higher prevalence of strokes and leukoaraiosis in patients with APS/SLE than in those patients with only SLE.
Vasculitis
A true cerebral vasculitis in SLE is rare, with a reported incidence in pathological studies of <10%.44 Clinical manifestations are highly variable, due to the potential of the inflammatory process to affect vessels of different sizes, and can range from mild cognitive impairment to severe neurological manifestations, including stroke, both ischaemic and haemorrhagic.12 The involvement of large vessels is extremely rare and has been associated with the most serious neurological manifestations and extremely high mortality rates.45,46
The main pathophysiological processes implied are the in situ formation or the deposition of immune complexes within the vessel wall and the action of antibodies against endothelial cells.13 Specifically, it has been shown that autoantibody binding to brain endothelial cell antigens can induce an endothelial activation eventually responsible for the vasculitic process.12
Other forms of SLE-related vasculitis can be drug-induced or infection-related, in the latter case either through direct damage of the vascular wall by micro-organisms or through antigen-induced autoimmune processes.13
Dissection
Arterial dissection is considered a very rare cause of ischaemic stroke; indeed, it has been reported that internal carotid artery dissection is responsible for <2% of all ischaemic strokes.47,48 Similar to other connective tissue diseases, SLE has a higher risk of vascular dissection. The pathophysiological correlation between SLE and arterial dissection is not clearly known. Many factors may play a role and can co-operate,49 determining a self-sustaining loop. Numerous factors are involved in the activation of autoinflammatory degeneration of vessel walls, such as endothelial and extracellular matrix damage, immune complex formation, and deposition.5,50
The chronic use of steroids induces arterial weakening and, along with hypertension, dyslipidaemia, and increased arterial stiffness, can lead to arterial wall dissection.
Despite the infrequent occurrence, when considering the possible aetiology of a SLE patient presenting with ischaemic stroke, the possibility of arterial dissection should be considered. Conversely, in a young patient presenting with stroke due to arterial dissection of unknown origin, it is mandatory to investigate a contingent coexistence of a rheumatic disease, such as SLE.51
HAEMORRHAGIC STROKE
Intracerebral Haemorrhage
IH in the SLE population is rarely reported in the literature.2,6,52,53 It has been shown that, compared to the general population, SLE patients present a 2–3-fold higher risk of IH, especially at younger ages.2,5,52
Several factors, most of which are also associated with ischaemic stroke, are implicated in the pathogenesis of IH in SLE. One of the most important is considered to be thrombocytopenia, diagnosed in >50% of affected patients, which can be secondary to different mechanisms, such as the administration of immunosuppressive agents, the presence of aPL antibodies, thrombotic microangiopathy, and bone marrow depression.54,55
Another important factor contributing to the high risk of IH in the SLE population is represented by the frequent use of anticoagulants to prevent thromboembolism events. This could also represent one of the reasons for the observation some authors have made that the longer the time from SLE diagnosis, the higher the relative risk of IH.6
The high prevalence of hypertension in the SLE population is another factor that is highly associated with a possible diagnosis of IH in these patients.27 Furthermore, vessel wall weakness, due to endothelial dysfunction or to a concurrent true vasculitic process, may be responsible for a major propensity of the vessel to rupture, thus causing IH.2,52 Eventually, the possibility of haemorrhagic transformation of an ischaemic infarction, especially after thrombolytic therapy, must also be considered.56
An interesting element confirming the more complex pathogenesis of IH in SLE patients in comparison with IH in the general population is the different anatomical localisation of the haemorrhages in the brain, which are often located in the cerebral lobes in the former group compared to the basal ganglia and internal capsule in the latter cases.52,57
Subarachnoid Haemorrhage
Several studies have showed a relatively frequent occurrence of SAH in SLE patients, with some authors reporting an up to 4-fold higher risk ratio and incidence rate compared to the general population.2,7
The causes of this increased incidence of SAH in SLE patients are not yet fully understood. Similar to the general population, rupture of intracranial aneurysms appears to be the most frequent cause of SAH in SLE patients.7 However, most of these aneurysms often present peculiar features; apart from the classic saccular (or ‘belly’) aneurysms, as in the general population, uncommon lesions, like distal fusiform aneurysms and multiple little aneurysms with atypical locations, are often described when SAH occurs in SLE patients.58 Furthermore, in some cases, SAH is not related to an obvious pathology, with no aneurysms or other pathological findings detected in the angiographic exams performed after SAH has occurred (the so called ‘angiogram-negative SAH’).58,59
Several pathophysiological hypotheses have been formulated to explain the higher incidence and the peculiar features of SAH in the SLE population. Once again, the increased prevalence of several traditional risk factors for SAH, especially hypertension and atherosclerosis, as well as endothelial damage, fibrinoid necrosis, and the activity index, represent key pathogenic factors for the onset of SAH, particularly for the greater likelihood of formation and rupture of classic saccular aneurysms.58,60
Cerebral vasculitis plays an important role too, especially in the genesis of atypical aneurysms; arterial inflammation causes lumen vessel narrowing and cerebral flow reduction, leading to ischaemia and haemodynamic stress, which are cofactors for aneurysmal genesis.7,61 Very little is known regarding the pathogenesis of angiogram-negative SAH. Treatment-related complications, especially for corticosteroid therapy, are likely to be involved in many of these cases.58,60 In fact, the use of a high daily dose of steroids has been shown to be an independent risk factor for an increased incidence of SAH.7,58
CONCLUSION
The risk of any stroke, whether ischaemic or haemorrhagic, is higher in SLE than the general population, especially in young individuals. Several traditional, potentially manageable risk factors, classically implicated in the genesis of stroke in the general population, play a critical role in the SLE population; for some of these risk factors, an increased prevalence has been noted in SLE patients compared to the general population. More attention and control of these factors (such as hypertension, diabetes, and anticoagulant dosage) are mandatory. However, classical risk factors alone fail to explain the higher incidence of stroke in SLE patients compared to the general population, especially when some elements are considered: the high incidence of stroke in people <50 years old, the higher CSVD score compared to patients with a previously occurring minor stroke, the high burden of atherosclerosis even after adjustment for traditional risk factors, the occurrence of atypical or rare events (e.g., dissection and atypical aneurysms). Although the precise pathophysiology responsible is not completely understood, several mechanisms have been hypothesised; in this context, inflammation and endothelial cell activation and damage play a crucial role.
Considering the high mortality and morbidity related to stroke and the young age of people involved, future studies focussing on the correlation between stroke and SLE are highly recommended, hopefully providing new insights into the treatment and prevention of vascular brain damage in these patients.








