It is unclear how long patients should be followed after radical prostatectomy (RP) for localised prostate cancer. The evidence is scarce, which relates to the fact that no studies have defined the risk of recurrence at an individual level. The risk of recurrence after RP is highly dependent on prostate specific antigen (PSA) level and tumour characteristics prior to and after surgery. Moreover, the risk is dependent on the length of follow-up, i.e. the risk declines the longer patients remain without recurrence. Also, in a population of patients who have undergone RP the risk of recurrence is affected by other events that may happen before, most importantly death due to other causes without recurrence. This must be accounted for when trying to describe the risk of recurrence in men undergoing surgery for prostate cancer.
We aimed to answer the question: ‘If a patient has been followed for X number of years after RP, remained alive and without recurrence, then what is the risk of recurrence in the future?’. To answer this, we developed a new and easily interpretable model to evaluate the risk of PSA recurrence after RP. The model was based on 1,970 consecutive patients who underwent RP from 1995–2013 with complete follow-up. PSA was measured six times within the first 2 years, then once annually. PSA recurrence was defined as the time from surgery to the first PSA reaching ≥0.2 ng/mL. The individualised risk of biochemical recurrence (BCR) was computed using multiple cause-specific Cox regression including preoperative PSA, primary Tumour (pT) category, RP Gleason score (GS), and surgical margin (R) status. Death without BCR was considered a competing event. The risks of BCR were dynamically updated by moving the time point of prediction in yearly intervals after RP. The risks of BCR within 1 year and within 5 years after the respective time point of prediction are reported. The median follow-up was 4.9 years. The individual risks of BCR were modified in the presence of risk factors. As an example, a patient with pT2, R negative status, GS 7 (3+4) on prostatectomy, a preoperative PSA ≤10 ng/mL, and 5 years of follow-up without BCR, had a predicted risk of BCR of 12% during the next 5 years (Figure 1). External calibration of the model is the primary limitation. The proposed estimates of the individualised risks of BCR during follow-up after RP appear as a new and useful tool when physicians and patients plan follow-up and PSA testing regimens after RP. The model is available as a free iOS-app, searchable under the term ‘CPC risk’.
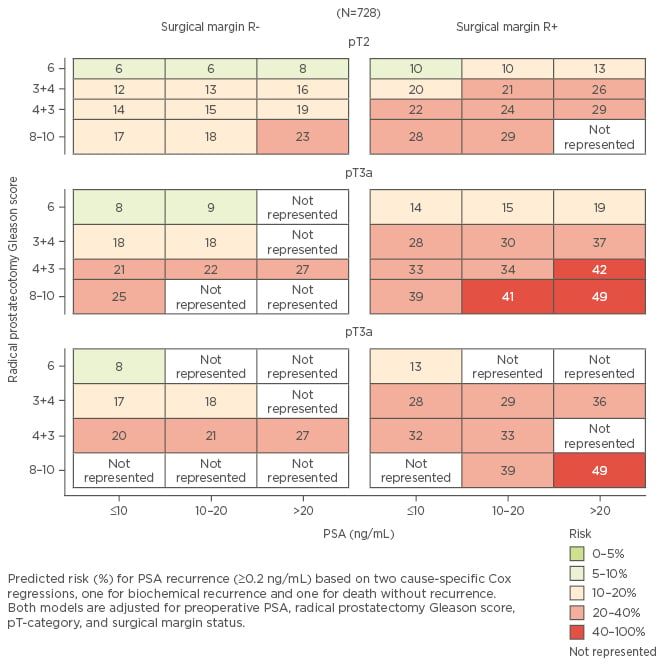
Figure 1: Risk of prostate specific antigen recurrence in the next 5 years after 5 years of follow-up.
The patients presented here are alive and without recurrence. ‘Not represented’ means that the specific patient group has either experienced recurrence or is no longer alive.
PSA: prostate specific antigen; pT: primary tumour; R: surgical margin status.








