Abstract
Zinner syndrome (ZS) is a rare urogenital condition characterised by the triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ipsilateral ejaculatory duct obstruction, resulting from malformation during early embryogenesis of the mesonephric (Wolffian) duct.
The authors present a 35-year-old male who was being evaluated for chronic hepatitis B virus infection. He was referred to the urology outpatient clinic on account of incidental ultrasound finding of solitary right kidney. General physical examination revealed a healthy-looking young male with a flat abdomen and no palpable enlarged organs. Digital rectal examination revealed normal sized prostate with no palpable pararectal masses. MRI of the pelvis revealed a triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ipsilateral ejaculatory duct obstruction.
The clinical diagnosis was asymptomatic ZS. He is on yearly follow-up at the urology outpatient clinic for lower urinary tract symptoms, pelvic pain, painful ejaculation, features of infertility, and pelvic ultrasound. If any of these symptoms occur, he will be treated with an α-adrenergic receptor blocker, drainage of the seminal vesicle cyst, and appropriate treatment for infertility. He is also on active surveillance for viral hepatitis by the gastroenterology team.
In conclusion, prompt referral and comprehensive radiological imaging investigations of patients with unilateral agenesis of the kidney will lead to increased identification and report of patients with ZS. There is paucity of literature reports on ZS in the authors’ environment, and this case report, to the best of the authors’ knowledge, is the first from Nigeria.
Key Points
1. The presence of a solitary kidney on incidental ultrasound evaluation should raise a high index of suspicion for Zinner syndrome (ZS).
2. CT scan and MRI are very important in establishing the diagnosis of ZS.
3. The association of infertility and ZS is not fully understood. Further study with close monitoring of ZS is likely to identify the exact cause of infertility, to provide appropriate pre-emptive treatment.
INTRODUCTION
Zinner syndrome (ZS) is a rare urogenital anomaly characterised by a triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst, and ipsilateral ejaculatory duct obstruction, which was first described in 1914 by Zinner.1 It arises from the abnormal embryological development of the mesonephric ducts occurring during the first trimester, and usually presents between the second and fourth decade of life, when there is an increase in the size of the seminal vesicle.2,3 Symptomatic patients often respond well to open surgical excision, transurethral deroofing, or laparoscopic excision of the seminal vesicles.4,5
The literature search did not reveal any publication from the authors’ environment; hence, the authors present this case report of asymptomatic ZS discovered in an asymptomatic chronic hepatitis B (HB) virus infection in a young male Nigerian, which, in the course of evaluating the liver by ultrasound, revealed a solitary right kidney. MRI further identified ipsilateral renal agenesis, ipsilateral cystic seminal vesicle, and ipsilateral ejaculatory duct cyst. In addition, teratozoospermia was observed in the seminal fluid analysis.
PATIENT INFORMATION
The patient was a 35-year-old, single factory worker, who first presented to the Urology outpatient clinic of the University College Hospital (UCH), Ibadan, Nigeria. He was the third of three children in a monogamous family setting. There was no family history of a similar medical condition, and he did not smoke or drink alcohol.
The patient was referred to Urology for evaluation of an incidentally noted congenital solitary right kidney during ultrasound evaluation of the liver, for the workup of chronic HB.
At the presentation, there were no upper or lower urinary tract symptoms, nor deep pelvic pain. There was no history suggestive of hypertension, diabetes, peptic ulcer, or bronchial asthma. There was no history of previous surgery and blood transfusion. He had been a patient of the Gastroenterology unit for 12 years on account of incidental HB surface antigen detection during a screening in school. He had remained asymptomatic on follow-up. HB e-antigen, HB e-antibody, and HB core immunoglobin M were all negative, and liver function test results were within normal limits.
Examination revealed a young man who was afebrile, not pale, anicteric, well hydrated, and with no demonstrable pitting pedal oedema. Vital signs were within normal limits. Chest, cardiovascular, abdominal, and external genitalia examinations were essentially normal. The digital rectal examination revealed a normal-sized prostate, and no other extra-rectal masses were felt.
The complete blood count, electrolyte urea, creatinine, and liver function tests were essentially normal. However, the semen analysis revealed teratozoospermia. The abdominopelvic ultrasound scan showed a normal urinary bladder and prostate, with dilatation of both the left ejaculatory duct and left seminal vesicle (Figure 1). The abdominal axial and coronal T1-weighted (T1W) MRI Fast Imaging Employing Steady-state Acquisition (FIESTA) images showed a normally located right kidney, and absent left kidney. The intestine was in the left renal bed, with the psoas muscle seen (Figure 2). Both pelvic axial T1W MRI and T2-weighted (T2W) MRIs showed cystic left seminal vesicles and a dilated left ejaculatory duct that were hyperintense on T1W images, and hypointense on T2W images, respectively (Figure 3).
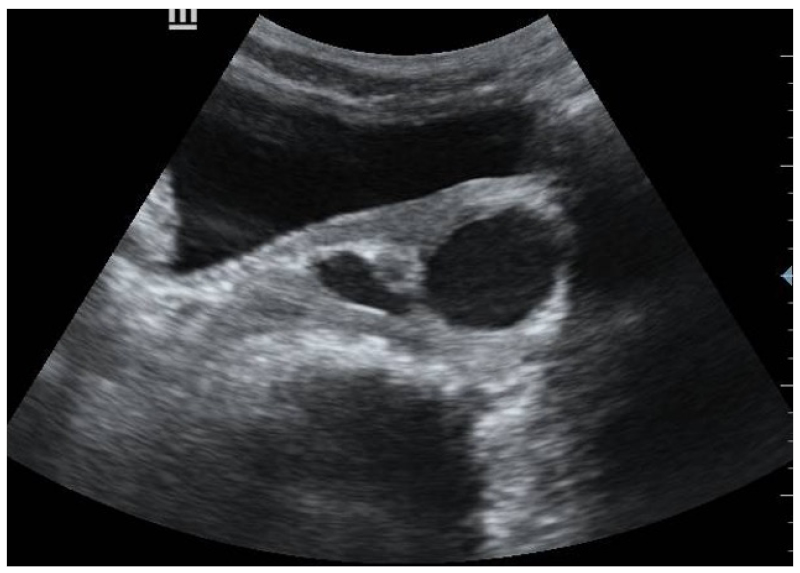
Figure 1: B-mode ultrasound images of patient with asymptomatic Zinner syndrome, showing left dilated ejaculatory duct and left seminal vesicle.
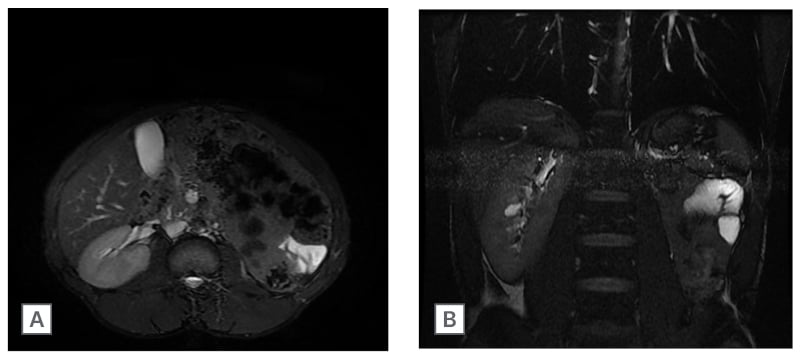
Figure 2: Fast Imaging Employing Steady-state Acquisition (FIESTA) MRI sequences.
A) Axial
B) Coronal
Scans show a normally sited right kidney with empty left renal bed; a bowel loop is noted as hyperintense structure surrounded by fat, just lateral to the left psoas muscle.
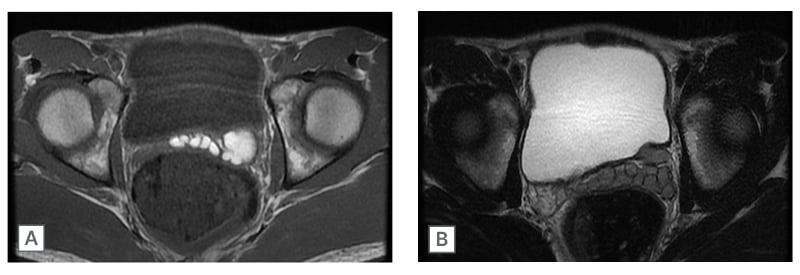
Figure 3: Pelvic axial MRI of dilated structure and adjacent beaded structures posterior to the urinary bladder.
A) T1W MRI showing hyperintense dilated structure and adjacent beaded structures posterior to the urinary bladder, all consistent with seminal vesicle cyst and ejaculatory duct dilatation.
B) T2W MRI showing the same structures, now hypointense.
The patient has remained asymptomatic and is currently on yearly follow-up with pelvic ultrasound to assess the growth rate of the seminal vesicle, as well as seminal fluid analysis for his fertility status.
The patient expressed surprise and was happy that his clinical diagnosis was identified, and promised to keep his appointment at the urology outpatient surgical clinic.
DISCUSSION
The triad of unilateral renal agenesis, ipsilateral obstruction of the ejaculatory duct, and ipsilateral seminal vesicle cyst, is referred to as ZS. The incidence of ZS is low. Sheih et al.6 reported that the incidence of seminal vesicle cystic dilatations in patients with ipsilateral renal agenesis or dysplasia was 0.0046% (13 in 28,000) among children in Taipei. Furthermore, van den Ouden et al.4 reported a pooled case of 52 cases of ZS before 1998.
In a systematic review of 214 cases of ZS between 1999–2020, Liu et al.7 reported that 80.8% of patients were symptomatic, with equal prevalence of right and left renal agenesis.
ZS is very rare among Africans. In their pooled study, van den Ouden et al.4 reported that only two patients (4%) were African. It is not surprising that only two cases have been reported from Africa to date.8,9 From these reports, it seems that there are racial differences in the reported incidence of ZS. In Ethiopia, Beyene et al.9 reported that a heightened sexual activity may have contributed to presentation in their case report. This has not been corroborated by other authors. The authors need to investigate this further in any new cases of ZS in Africa.
This geographical question could be answered by screening preschool children and adults for renal agenesis with abdominal ultrasound, before entry into secondary schools or tertiary institutions. This may likely increase the reporting of ZS in Nigeria, and across Africa. Of note is the presentation of incidental solitary right kidney in this case report, picked up on ultrasound. This is the first case report from Nigeria that was asymptomatically discovered while evaluating this index patient for asymptomatic chronic HB infection. Further evaluation of the patient was based on a high index of suspicion for ZS. With this case report from Nigeria, the authors hope to raise clinicians’ level of awareness, and encourage them to thoroughly evaluate any case of ipsilateral renal agenesis in order to identify the full spectrum of congenital anomalies in such patients. This may translate into higher incidence of a condition that has seemingly been under-reported or misdiagnosed in Nigeria.
A study in China, where ZS is also rare, discovered genetic features in the 14 cases reported. The mutated genes were BMP4, RPGRIP1L, SEC63, SETD2, AGFG1, FLT1, and ZNF141.10 The authors cannot categorically state that there is a genetic impact on ZS from this case report. However, they could explore this possibility by screening for the mutated genes in their patient, to determine genetic features in patients with ZS in Africa.
The aetiology of ZS is believed to result from the developmental arrest of the mesonephric (Wolffian) ducts during the fifth week of embryogenesis. This is particularly obvious since the mesonephric duct in males develops to form half of the trigone, the urinary bladder neck, urethra, seminal vesicle, vas deferens, epididymis, and epididymal heads, under the influence of testosterone and Müllerian duct inhibitory factor. Thus, the outcome of such disturbances includes ipsilateral renal agenesis, dilatation of the distal ureter, cystic dilatation of the seminal vesicle, and obstruction of the ejaculatory duct on the affected side.4,11
The clinical presentations of ZS are variable and non-specific, often leading to diagnostic challenges.10,12 Many patients tend to become symptomatic between the second and fourth decade of life, when there is an increase in the size of the seminal vesicle to >5 cm.3 Some common presentations in ZS include lower urinary tract symptoms, such as urinary frequency and pelvic pain.12,13 The indications for surgical intervention are recurrent urinary tract infections,14 and haematospermia.15 ZS is a recognised cause of painful ejaculation and male infertility.16,17 The patient in this case report had a significant percentage of abnormal sperm cells, despite good sperm concentration and motility; therefore, he should be closely monitored.18 The complete blood count, electrolytes, urea, and creatinine, as well as liver function test, and serum prostate-specific antigen, were essentially normal.
MRI is the gold standard in the diagnosis of ZS. It is often performed in the coronal and transverse plane without contrast. The protocol commonly used is T1W turbo spine-echo (TSE), T2W TSE, and a T1W TSE fat-saturation. It often shows a multiloculated seminal vesicle cyst that is hypointense on T1W images, and appears bright on T2W images. The MRI features are renal agenesis and occasional situs inversus viscerum, as well as lobulated multiloculated cystic lesion of the seminal vesicle with saccular dilated enlarged ectopic ureter that opens into the cystic seminal vesicle. This is well appreciated in the T1W coronal view.19,20
Contrast-enhanced axial CT of the abdomen with coronal reconstruction shows ipsilateral renal agenesis, and lobulated multiloculated cystic seminal vesicle with saccular dilated, with or without enlarged ectopic ureter, that opens into the cystic seminal vesicle. The dilated seminal vesicle does not demonstrate contrast enhancement, which is in keeping with non-malignant cyst.19,20
Abdominal ultrasound shows solitary kidney and empty contralateral renal bed with a retrovesical liquid mass. Transrectal ultrasound visualises retrovesical hypoechoic cyst with posterior enhancement and impure content that compresses the urinary bladder, and protrudes into the bladder lumen.14,21 However, in environments with limited resources, abdominal CT or ultrasound scan are suitable alternatives to MRI.14,20
Seminal fluid analysis is also an important investigation in ZS, as about 45% of cases are documented with infertility.22 In some cases, cystoscopy may be necessary to exclude ipsilateral ejaculatory duct causing bladder outlet obstruction, as this may require aspiration.23
Observation with close follow-up is advocated for those who are asymptomatic, as in this case report. The duration of follow-up needed is variable, and the longest documented follow-up is that reported by Kelly et al.,24 where the patient was followed up for 14 years, and eventually had a successful laparoscopic excision of his increased seminal vesicle cyst. Other available treatment options of seminal vesicle cysts include open or robotic excision of the cysts.25,26
In cases with infertility and painful ejaculation, transurethral resection of ejaculatory ducts aid resolution of symptoms, and improve semen characteristics.4
CONCLUSION
This case report from Nigeria will increase the level of suspicion from ultrasound screening, encourage thorough evaluation of patients with solitary kidney, and reduce misdiagnosis and under-reporting of ZS. Asymptomatic patients should be closely followed up with imaging studies and laboratory tests, and appropriately treated when symptomatic.







