Abstract
Objective: Hypospadias is one of the most common congenital anomalies of male genitalia and is usually repaired in the first 2 years of life. Regarding distal forms of hypospadias, however, controversies surrounding the need for surgical repair may lead to delayed referral secondary to symptoms. This article reviews the authors’ experience in boys who presented with symptoms secondary to an untreated distal hypospadias.
Materials and methods: The authors reviewed their prospectively maintained database and included all children who were secondarily referred because of symptoms due to untreated distal hypospadias in the last 5 years. The data were reviewed and analysed.
Results: Seventeen patients were identified. The median age at referral was 118 months. Symptoms at presentation included poor stream, straining during voiding, incontinence, and unhappiness related to cosmesis. Surgical correction included meatoplasty or tubularised incised plate urethroplasty. The choice between foreskin reconstruction or circumcision was based on parental preference.
Conclusion: The authors have presented a cohort of children with untreated distal hypospadias associated with functional and cosmetic problems. Both could be underestimated at birth, leading to problems in late childhood. Viewing repair of distal hypospadias as a purely cosmetic surgery is to disregard the nature of the anomaly and its associated implications.
INTRODUCTION
Hypospadias is one of the most common congenital abnormalities of male external genitalia with an incidence of 1 in 200–300 live male births, and its correction represents a common surgical procedure performed by paediatric urologists.1,2 Based on the severity and the location of the meatus, hypospadias is classically divided into proximal, mid-shaft, and distal forms, with the latter accounting for 70–80% of cases.3 Indications for undergoing a surgical repair are mainly related to function and cosmesis.
Distal forms are often labelled as ‘functionally normal’ and therefore their repair is debated.4 While, in general, babies born with hypospadias are referred to specialist services and operated on within the first 2 years of life, parents of children with distal hypospadias are sometimes reassured that no functional impairment is associated with this defect. As a result of this reassurance, no referral is made, leaving the child with an untreated hypospadias. The symptoms of untreated hypospadias primarily include a downward deflected urine stream, dysuria, and urinary incontinence.
The authors aimed to review the children referred to their department with hypospadias, focussing on late referral of children with untreated distal hypospadias.
MATERIALS AND METHODS
The authors reviewed their prospectively maintained database for all hypospadias patients referred to their unit. They collected data for all patients with distal hypospadias referred over the last 5 years (from January 2014–December 2018), including all children who were secondarily referred with symptoms related to an untreated distal hypospadias. The authors considered all children who presented to them with symptoms related to their hypospadias after 3 years of age. These patients were previously seen by other healthcare professionals (paediatricians and group practice); the authors defined this as late referral. Patients who had a previous hypospadias repair and presented at a later age with complications were not included.
The patients’ referral letters, medical notes, assessments, and operation documents were reviewed. Symptoms at presentation, clinical findings, and the procedures performed were recorded and evaluated.
RESULTS
In the analysed period, the authors identified 17 patients who presented with symptoms secondary to an untreated distal hypospadias. Patient characteristics are set out in Table 1.
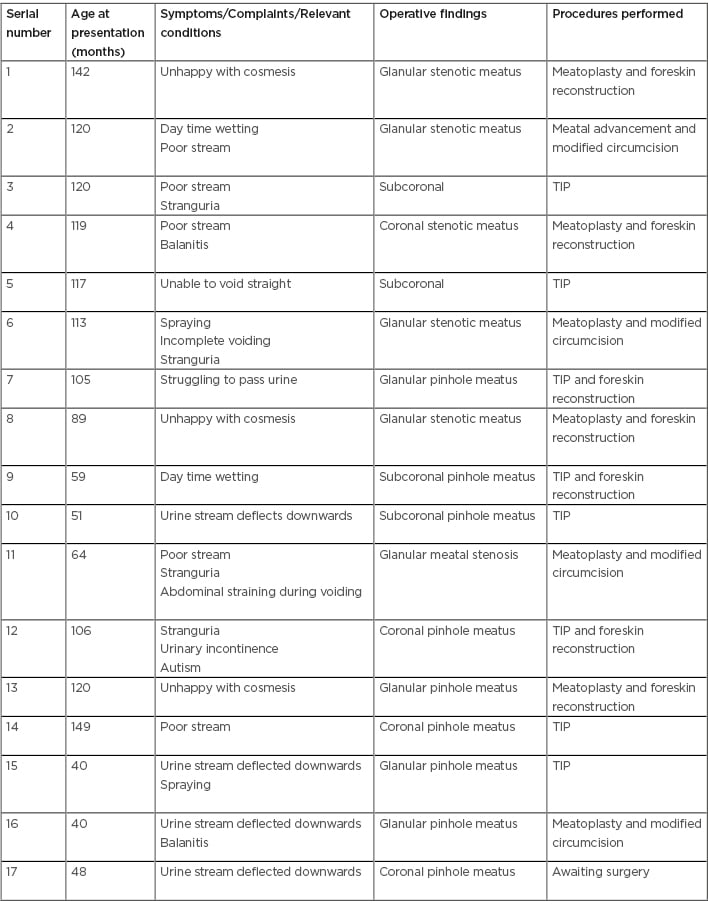
Table 1: Patient characteristics.
TIP: tubularised incised plate urethroplasty.
The median age at referral was 118 months (range: 40–149 months). Three boys (Patients 1, 8, and 13) were asymptomatic but unhappy with the cosmesis. The remaining children (n=14) presented with symptoms. Common symptoms reported were poor stream, straining during voiding, and daytime wetting.
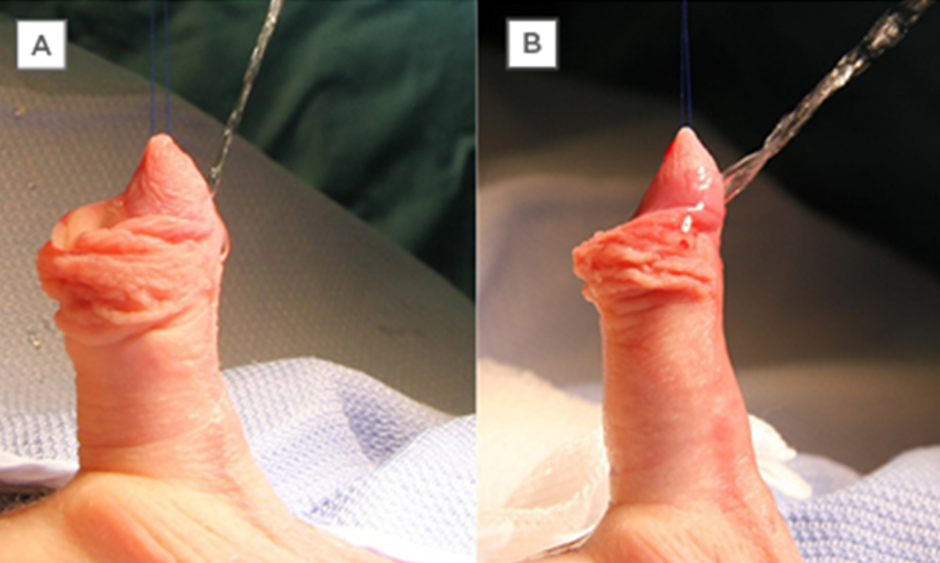
In nine boys, the meatus was glanular and, in the remainder, the meatus was either coronal or subcoronal. All patients with glanular hypospadias who were found to have meatal stenosis were offered a meatoplasty. Patients with coronal and subcoronal hypospadias underwent a tubularised incised plate urethroplasty. Depending on parental preference, the foreskin was either preserved and reconstructed (n=7) or removed (n=9) (Patient 17 is currently awaiting surgery). Most children presented with a stenotic meatus (Figure 1) and a narrow stream (Figure 2A). In these children, a preoperative uroflow study showed a plateau curve suggesting an obstructed flow (Figure 3). The authors did not conduct any ultrasonography in any patients. Some of the children who presented with daytime (and night-time) wetting reported having previously failed the classic management strategies for treating urinary incontinence.5
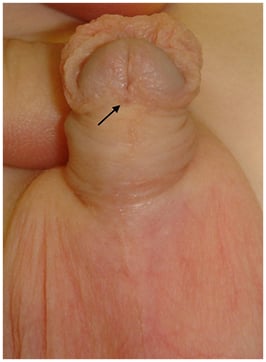
Figure 1: Preoperative image of an untreated hypospadias.
The arrow points to the pin-hole coronal meatus.
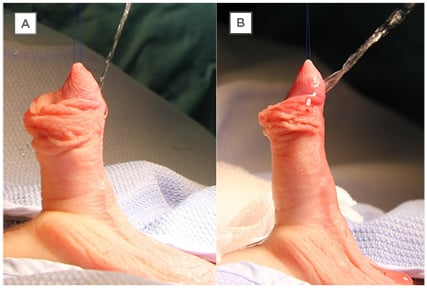
Figure 2: A) Shows the stream assessed intra-operatively before meatoplasty and B) after meatoplasty.
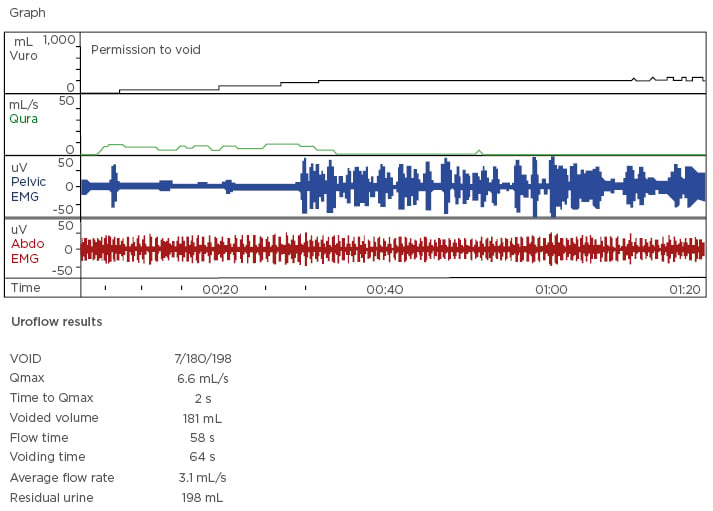
Figure 3: Shows uroflow in patient with meatal stenosis. The Qmax is 6.6 mL/s with a plateau shaped curve suggesting obstructed flow.
EMG: electromyography; Qmax: maximum flow rate.
In particular, as an example, before being referred to the authors’ unit, Patient 2 underwent many assessments and medical treatments (including being referred to a psychologist) to correct what was considered to be primary urinary incontinence. His symptoms completely resolved following the operation. In another boy (Patient 12), who was still in nappies at the age of 8 years, the incontinence was considered secondary to mild autistic condition, thus the parents were told that no solution was available, and potty training was not possible.
DISCUSSION
Repair of distal hypospadias, despite being a commonly performed procedure by paediatric urologists, is still a controversial matter. Many aspects of the treatment are debated, such as the fate of the foreskin,6 the need for postoperative stenting7 or for antibiotic prophylaxis,8 and, ultimately, whether it should be considered as a functional or cosmetic repair.4,9
In a recent editorial, Snodgrass and Bush9 argued that distal hypospadias repair should not be considered a cosmetic operation. The authors agree with this and believe that the presented series could represent further supporting evidence for that position.
A penis affected by hypospadias is not developed normally and if the condition is left untreated, it can be associated with multiple symptoms.9 The symptoms are primarily due to the presence of an abnormal meatus and include voiding with a downward deflected urine stream, dysuria, strangury, and urinary incontinence.10,11
Similar to some of the authors’ patients, in a series published in 2009, an obstructive urinary flow pattern was observed preoperatively in 25% (16 out of 63) of patients with hypospadias who were aged 5–11 years. In one-third of them, the presence of meatal stenosis was then confirmed intraoperatively.12
Similar observations were also reported by Oslen et al.,13 who found low maximum flow rates with plateau shaped curves in 31% of infants with hypospadias. Presence of a meatal narrowing is a reported cause of urinary symptoms, as identified in some of the authors’ patients. If it goes undetected or underestimated, it could lead to unnecessary treatments and major distress.14,15
Cases like the two children mentioned above, where their incontinence was considered primary or related to autism, should never occur and could have simply been avoided by a thorough physical examination and an appropriate early referral to a paediatric urologist.
Only a few reports are available about patients with uncorrected hypospadias. Fichtner et al.,4 in a study conducted in 500 men, found a 13% incidence of distal hypospadias (glanular, coronal, and subcoronal). Of these, 63% reported being unaware of any penile abnormality and that they had a normal sexual history. The authors also pointed out that these patients were able to void in standing position with a straight and single stream, concluding that the repair of distal hypospadias should be considered a cosmetic surgery. Similarly, in a report by Dodds et al.,16 in a cohort of 56 adults with hypospadias (9 of those with previous failed surgical repair and 47 untreated), it was suggested that many of them appeared to have adapted to their congenital anomaly without any surgical correction.
However, a different message is provided in a survey reported by Schlomer et al.17 They recruited 736 adult men who completed an online questionnaire regarding penile self-anatomy; of these men, 52 (7.1%) self-identified as having a possible untreated hypospadias. Among all responders, men with a possible untreated hypospadias reported adverse outcomes compared to normal men. The most significant adverse outcomes appeared to be the presence of penile curvature and difficulty with intercourse caused by the penile curvature.
Furthermore, as reported by Snodgrass and Bush in their editorial,9 a survey performed by Keays et al.10 showed that 37% of uncorrected hypospadias patients had a deviated stream and only 39% could void straight. In addition, 54% were dissatisfied with their voiding, with 29% being very dissatisfied. This survey also covered patients’ satisfaction regarding cosmesis and reported that 33% of men with uncorrected hypospadias were dissatisfied with penile appearance, 41% were worried about “what others would think about it,” and 46% reported being teased because of it.10 In the current series, despite the absence of functional problems, 3 boys expressed their dissatisfaction regarding the cosmesis and requested a surgical intervention.
A possible argument against early correction of distal hypospadias could be the perception that delaying the decision would save parents from having to be responsible for making a decision on their son’s behalf and could reduce the risk of parental regret.18,19 Although this view is understandable and could be considered, it should not be implemented if the consequence carries the risk of years of suffering and embarrassment.10 A study from Nigeria20 quoted two peaks of age at surgery. One peak was noted in the age group of 1–3 years and the second peak at 5–10 years. They noted that chordee was the most common problem associated with hypospadias. The authors cited problems with paediatric anaesthesia resulting in the later age group for surgical correction.
Surgical correction of distal hypospadias carries minor risks, but outcomes in the majority of cases are successful and, despite some variations among different techniques, complication rates are relatively low.21-23 In view of the presented case series, the authors believe that correction of distal hypospadias is not a cosmetic surgery and would recommend that all children with hypospadias, regardless of the severity, should be referred to a specialist paediatric urologist. This will provide the child with the best possible assessment to identify those at risk of developing functional issues (those with a pinhole/stenotic meatus) and will give parents the option to be appropriately counselled regarding the risks and benefits of surgical and conservative management.
CONCLUSION
Distal hypospadias can be associated with both functional and cosmetic problems that may be underestimated at birth and generate symptoms at an older age. Repair can be safely achieved with minimal risk of complications and can easily be performed in infancy, thereby avoiding problems which can develop later in life. To consider the repair of distal hypospadias as a purely cosmetic surgery is to disregard the nature of the anomaly and its associated implications.