Abstract
Introduction: Non-high-density lipoprotein (non-HDL) cholesterol is the sum of low-density lipoprotein (LDL) cholesterol and very-low-density lipoprotein (VLDL) cholesterol, and is usually approximated by the total cholesterol minus HDL-cholesterol. The National Lipid Association (NLA) has advocated the use of non-HDL cholesterol as its favoured lipid predictor. Cut-off points are based on LDL cholesterol values, with a lower end at 100 mg/dL (2.50 mmol/L) and a higher end at 190 mg/dL (4.75 mmol/L), adding 30 mg/dL (0.75 mmol/L) to keep triglyceride (TG) levels <150 mg/dL (1.70 mmol/L).
Objectives: The author will demonstrate that the use of non-HDL cholesterol has not been fully considered.
Methods: The author will examine a general population lipid database to demonstrate the frequency of distribution of non-HDL cholesterol in the part of the population that was known to have developed a form of atherothrombotic disease (ATD) and in the part that was not known to have done so. The effect of stratifying each non-HDL cholesterol quintile in terms of another lipid predictor that does not involve VLDL-cholesterol or TG will be demonstrated. The other risk predictor is the cholesterol retention fraction (CRF) defined as (LDL-HDL)/LDL.
Findings: All non-HDL cholesterol quintiles above the lowest quintile had higher frequencies in the ATD population than in the non-ATD population. The highest two quintiles had frequencies in the ATD population that are 2.5-times as high as those in the non-ATD population, whereas in the middle two quintiles, the frequency in the ATD population was minimally higher than in the non-ATD population. In the lowest quintile, the frequency is much higher in the non-ATD population than in the ATD population. At any non-HDL cholesterol quintile, the average age of ATD onset depends on cigarette smoking (not discussed here) and the CRF. Higher CRF levels equate to an earlier average age of ATD onset and lower levels of CRF equate to a later onset. A 75-year-old male who was a hypertensive diabetic and a former smoker was not on statins because of low lipid levels, had clean arteries on angiography, whereas a 45-year-old normotensive, non-smoking patient with severe dyslipidaemia (obtained at first encounter) had a massive stroke due to carotid stenosis. Both had non-HDL cholesterol levels in the intermediate ATD risk quintiles.
Conclusions: Non-HDL cholesterol is not the optimal predictor of the population at risk of atherothrombotic disease and its use should be reconsidered.
INTRODUCTION
The National Lipid Association (NLA) has recently advocated non-high-density lipoprotein (non-HDL) cholesterol as a prime lipid predictor for the prediction of the population at risk of atherothrombotic disease (ATD).1 Non-HDL cholesterol is the sum of the low-density lipoprotein (LDL) cholesterol and the very-low-density lipoprotein (VLDL) cholesterol. Non-HDL cholesterol can also be approximated by total cholesterol (TC) minus HDL cholesterol.
While the concept of non-HDL cholesterol is not new, there are no randomised controlled clinical trials to validate non-HDL cholesterol as either a lipid predictor or a guide to the treatment of dyslipidaemia to stabilise/regress plaque or decrease ATD events. Non-HDL cholesterol was mentioned in the write-up of the Helsinki Heart Study but, as the authors stated, the aim of the study was to prove the lipid regulatory hypothesis of Dr Esko Nikkila, which stated that maximal regression of atherosclerosis occurs when LDL cholesterol is lowered simultaneously with HDL cholesterol being raised.2
The purpose of this paper is to discuss the limitations of non-HDL cholesterol in terms of the Bowling Green Study (BGS) database. The author will show that non-HDL cholesterol is a suboptimal predictor compared with the cholesterol retention fraction (CRF) (defined as [LDL-HDL]/LDL) and that the use of non-HDL cholesterol as a lipid predictor should be reconsidered.
MATERIAL AND METHODS
The author established the BGS of the primary and secondary prevention of ATD initially as a means of predicting the population at risk of ATD, and subsequently as a guide to the maximal stabilisation/regression of plaque and maximal reduction of ATD events.3-5 When establishing the BGS, the author created an age-sex database of all patients in his practice who had had a lipid profile during the BGS study timeframe of 4th November 1974–4th November 2003. During the years prior to 1st January 1978, only TC and triglyceride (TG) levels were available, but in the years following 1st January 1978, HDL cholesterol and LDL cholesterol were also available. HDL cholesterol was measured by the precipitation method and LDL cholesterol was calculated by the Friedewald formula.6 Since LDL cholesterol calculations are relatively accurate above 400 mg/dL (4.5 mmol/L), the author accepted LDL cholesterol calculations up to TG levels of 500 mg/dL (5.6 mmol/L).7 This point may be controversial, and indeed the author spoke to Dr Friedewald a number of years ago on this matter. Dr Friedewald insisted that his formula should not be used when TG levels exceeded 400 mg/dL (4.5 mmol/L). However, Wilson et al.7 have shown that LDL cholesterol calculations are relatively accurate in the 400–500 mg/dL (4.5–5.6 mmol/L) region and the author has elected to follow WIlson et al. in this matter so that more CRF determinations are available. Two-hour postprandial blood sugar levels were also obtained in most cases of lipid screening. Cigarette smoking status was not routinely ascertained until 1984, when it became clear that cigarette smoking played a fundamental role in the pathogenesis of ATD events. Blood pressure determination, height, and weight were measured at every office visit, and BMI was calculated on the initial visit and periodically thereafter.
The author’s practice of family medicine in northwest Ohio is located in Bowling Green, the county seat of Wood County. Wood County is largely a rural county, with many professional occupations in agriculture and small businesses. The largest employer is Bowling Green State University and the population of Wood County was about 128,000 at the time of the last census, of which about 30,000 live in Bowling Green. The population is mainly Anglo-Europeans in ancestry and the chief minority group is Latin American. African-Americans and Asian-Americans are not present in large numbers.
Risk factors for ATD were not well understood in the 1970s and 1980s and because many dyslipidaemic patients refused therapy or had an inadequate response to therapy, a number of the author’s patients developed some form of ATD. The BGS was not a randomised controlled clinical trial. All dyslipidaemic, hypertensive, and diabetic patients were offered therapy; some accepted, but many declined. All cigarette smokers were advised to quit smoking.
All known ATD risk factors were examined, including dyslipidaemia, cigarette smoking, hypertension, diabetes mellitus, obesity, age, sex, and occasionally a hypercoagulable state. In searching for the best lipid predictor, the author noted the promotion of the Framingham Fraction (TC:HDL) but declined its use since it was based on non-fasting blood. However, in 1981, an article was published asking if the LDL:HDL ratio was the best lipid predictor. From this suggestion was born the concept of the CRF (defined as [LDL-HDL]/LDL), which sought to determine what percentage of cholesterol entering the artery stays within the artery wall. After evaluation, the BGS determined the CRF to be its best lipid predictor.8
The determination of the population developing some form of clinical ATD was based on clinical findings. For example, acute myocardial infarction (MI) was based on the acute onset of typical mid-sternal chest pain (described as a pressure, heaviness, or an ache, with or without radiation) and was virtually always accompanied by electrocardiographic and/or cardiac enzyme changes. Sudden unexpected death was included within the MI category. On the other hand, angina pectoris displayed a similar pain without electrocardiographic/enzyme changes, and was of a chronic, recurrent nature. A stroke was diagnosed in patients with acute neurologic changes, either sensory or motor, lasting ≥1 hour. A transient ischaemic attack had similar findings, but those findings had to be resolved within 1 hour. Aneurysms were generally found on radiographic testing. About 40% of patients presented with a history of an ATD event, and in such cases the author attempted to authenticate the diagnoses, though often this was not possible.
RESULTS
In the BGS population database, the frequency distribution of non-HDL cholesterol is determined in terms of biological sex and in terms of the frequency of each quintile in the ATD and non-ATD populations, using the quintiles suggested by the NLA (Table 1). It will be noted that the quintiles given in this paper are different than those recommended by the NLA. The reason for this is that the manufacturers of the auto-analysers changed the methodology by which they measured HDL cholesterol. The older precipitation method of HDL cholesterol measurement was the gold standard utilised by laboratories worldwide and was the method used to measure HDL cholesterol in all of the atherosclerosis regression studies conducted prior to the year 1999. The newer enzymatic method has been used in most of the atherosclerosis regression studies undertaken since the year 1999. The two methods give differing values for HDL cholesterol: the value obtained using the enzymatic method is an order of 10 mg/dL (0.26 mmol/L) higher than that obtained using the precipitation method. Consequently, the calculated LDL cholesterol using the enzymatic method will be in the order of 10 mg/dL (0.26 mmol/L) lower than that obtained using the precipitation methodology.9 This makes the comparison of databases obtained before and after the methodology conversion difficult unless a conversion factor is utilised. For this study, the conversion factor is: HDL cholesterol (precipitation method)=(HDL cholesterol [enzymatic method] minus 12)/0.93.
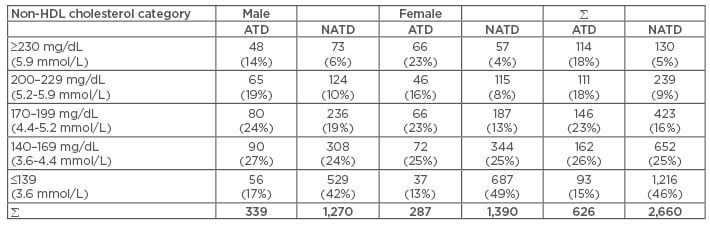
Table 1: Non-high-density lipoprotein cholesterol distribution in Bowling Green Study atherothrombotic disease population versus non-atherothrombotic disease population 1974–2003.
The freestanding number in each column represents the actual number of patients. The number in parentheses represents the percentage of the group (column). Non-HDL cholesterol categories based on BGS equivalences. To determine comparative NLA values, subtract 10 mg/dL (0.26 mmol/L).
HDL: high density lipoprotein; BGS: Bowling Green Study; ADT: atherothrombotic disease; NATD: non-atherothrombotic disease.
The NLA guidelines for non-HDL cholesterol are based on LDL cholesterol goals, with the upper-most quintile being defined by the LDL cholesterol level establishing familial hypercholesterolaemia (i.e. 190 mg/dL [4.9 mmol/L]) and the lowest quintile defining an optimal LDL cholesterol level, at which little LDL cholesterol enters the artery wall (i.e. 99 mg/dL [2.6 mmol/L]). The non-HDL cholesterol values in between these two extremes were divided into three groups to make up the other three quintiles. The NLA then added 30 mg/dL (0.77 mmol/L) to each quintile to correct for the cholesterol carried by VLDL.
The BGS database was compiled mainly before the HDL cholesterol measurement conversion and hence its regional laboratory utilised the precipitation methodology. As a result, a LDL cholesterol value (using the enzymatic methodology) of 190 mg/dL (4.5 mmol/L) is equivalent to a LDL cholesterol of 200 mg/dL (5.2 mmol/L) in the BGS database. Similarly, a LDL cholesterol (using the enzymatic methodology) 100 mg/dL (2.6 mmol/L) is equivalent to a LDL cholesterol of 110 mg/dL (2.8 mmol/L) in the BGS database. Adding the 30 mg/dL (0.77 mmol/L) to each number gives the results depicted in Table 1.
The non-HDL cholesterol quintiles depicted in Table 1 can be graded into ATD risk categories on the basis of frequencies within the ATD and non-ATD populations. The frequency of the two highest quintiles (>200 mg/dL [5.2 mmol/L]) in the total ATD population was 36% (225/626) and in the total non-ATD population was 14% (369/2,660). Since the frequency of the two highest quintiles in the ATD population was about 2.5-times as high as in the non-ATD population it is reasonable to attribute the highest ATD risk to these two quintiles, though in a graded fashion. Similarly, the frequency of the middle two non-HDL cholesterol quintiles in the ATD population was 49% (308/626) and 40% (1,075/2,660) in the non-ATD population. There appears to be a graded intermediate ATD risk for non-HDL cholesterol in the 140–199 mg/dL (3.6–5.2 mmol/L) range. On the other hand, the frequency of the lowest quintile of non-HDL cholesterol in the ATD population was 15% (93/626) and 46% in the non-ATD population.
The range of CRF values in any given non-HDL cholesterol quintile is widely variable. Table 2 shows the average ages of ATD onset for each CRF-non-HDL cholesterol cohort in the BGS ATD population. The data clearly showed that at any quintile of non-HDL cholesterol, the average age of ATD onset is determined by the associated CRF value, with earlier ages of ATD onset occurring when CRF levels are higher and later ages of ATD onset occurring when CRF values are lower, in a linear fashion. The converse is not true: at any level of CRF, non-HDL cholesterol does not predict the average age of ATD onset. These findings are also true for LDL cholesterol.
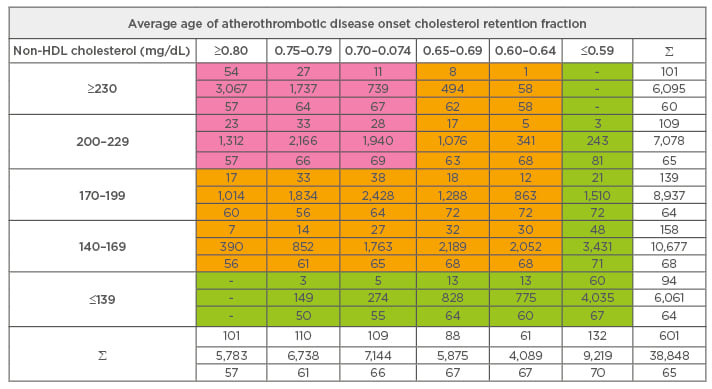
Table 2: Cholesterol retention fraction distribution in non-high density lipoprotein cholesterol atherothrombotic disease Bowling Green Study General Population: 1974–2003.
Non-HDL: non-high-density lipoprotein.
Using the BGS database, a table can be set up for both CRF and non-HDL cholesterol, placing the highest risk cohorts in the ‘red’ zone, intermediate risk cohorts in the ‘yellow’ zone, and the lowest risk cohorts in the ‘green’ zone. The highest risk zone for CRF is ≥0.70; the intermediate risk zone, 0.60–0.69; and the lowest risk zone, ≤0.59. For non-HDL cholesterol, the highest risk zone is ≤200 mg/dL (5.2 mmol/L); the intermediate risk zone, 140–199 mg/dL (3.6–5.2 mmol/L); the lowest risk zone, ≤139 mg/dL (3.6 mmol/L). The result of this analysis can be seen in Table 3. At any risk zone of non-HDL cholesterol, the risk zone for the CRF determines the average age of ATD onset. (The red zone parameters for the enzymatic method of HDL cholesterol measurement and the NLA quintiles are CRF of 0.60 or higher and non-HDL cholesterol of 190 mg/dl [5.1 mmol/L]; the yellow zone, CRF=0.50–0.59 and non-HDL cholesterol= 130–189 mg/dL [3.4–5.1 mmol/L]; the green zone, CRF of 0.49 and lower and non-HDL cholesterol of 129 mg/dL [3.4 mmol/L] or lower).
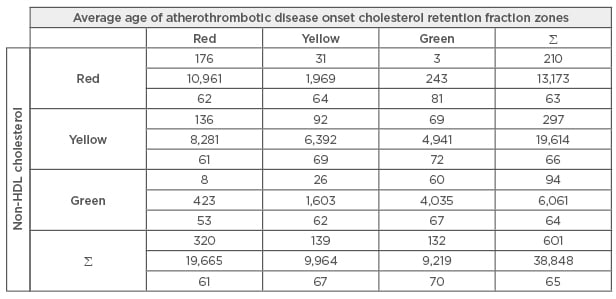
Table 3: Cholesterol retention fraction versus non-high-density lipoprotein cholesterol the Bowling Green Study general population: 1974–2003.
Non-HDL: non-high-density lipoprotein.
The author would like to make note of a comparative case that occurred in his practice. A 75-year-old male, who was an insulin-dependent diabetic, hypertensive, former smoker with acceptable lipids (TC=189 mg/dL [4.9 mmol/L], HDL cholesterol= 36 mg/dL [0.9 mmol/L], LDL cholesterol=110 mg/dL [2.8 mmol/L], TG=214 mg/dL [2.4 mmol/L], non-HDL cholesterol=153 mg/dL [4.0 mmol/L], and CRF=0.67) at 43 years of age, further LDL cholesterol lowering occurring naturally over the subsequent years. His lipids were followed over time as the author followed the patient’s blood sugar level and blood pressure; since his LDL cholesterol fell to very low levels, the patient was not placed on a statin. At 75 years of age the patient needed to have orthopaedic surgery and cardiac clearance was requested. An angiogram was performed and his coronary arteries were found to be devoid of plaque. Another patient who came into the author’s practice at the age of 45 years, having suffered a massive stroke due to carotid stenosis, had avoided seeing physicians in the belief that he was doing well. He had never smoked cigarettes and had his blood pressure taken with good results: 120/80 mmHg. He also had a TC with a value of 200 mg/dL (5.2 mmol/L). The author attended the patient in the casualty department of the local hospital and obtained a full lipid profile, which was abnormal: TC=200 mg/dL (5.2 mmol/L), HDL cholesterol=25 mg/dl (0.6 mmol/L), LDL cholesterol=145 mg/dL (3.7 mmol/L), non-HDL cholesterol=175 mg/dL (4.5 mmol/L), and TG=150 mg/dL (1.7 mmol/L). His CRF was 0.83. The non- HDL cholesterol values for both patients were in the intermediate risk range, yet in the former patient, statin therapy was held as the author followed the patient’s lipids and when the LDL cholesterol fell of its own accord, never initiated since the CRF fell below 0.59 (precipitation method but 0.49 using the enzymatic method), whereas the patient who had the stroke had a CRF that demanded immediate treatment long before his acute ATD event.
DISCUSSION
Non-HDL cholesterol represents the sum of all of the apolipoprotein (apoB) carrying particles in the blood, and hence has been referred to as the new atherogenic dyslipidaemia.1 Non-HDL cholesterol has been advocated as a first-line lipid predictor by the NLA. This position is based on numerous studies, usually comparing non-HDL cholesterol with LDL cholesterol or apoB.10-19 Non-HDL cholesterol has been advanced as a surrogate for apoB20 but may in fact be superior to apoB in predicting the population at risk of ATD.21,22
The use of lipid ratios was first suggested by Kannel et al.23 in 1979, describing the findings of the Framingham Heart Study.23 Initially advocated was the ratio between TC and HDL cholesterol (TC:HDL). Since the bulk of lipid profiles at that time were performed on non-fasting blood, LDL cholesterol calculations were not available to Kannel et al. Some studies, done with fasting blood, have proposed the apoB/apoA-1 ratio instead.24-26 The apoB/apoA-1 ratio has not been shown to be superior to non-HDL cholesterol as a predictor27-29 and non-HDL cholesterol has not been shown to be superior to TC: HDL.30 Other studies have compared the predictive abilities of the LDL:HDL cholesterol ratio to apoB, and the ratio is superior to apoB.31
Elshazly et al.32 have analysed eight intravascular ultrasound studies involving 4,917 patients and found that the TC:HDL cholesterol ratio was a better predictor of plaque stabilisation/regression and major adverse cardiovascular events than LDL cholesterol, non-HDL cholesterol, and apoB. This finding adds to the author’s call to use lipid ratios in the evaluation of ATD risk and to guide therapy to maximally stabilise/regress atherosclerotic plaques.33
The author has advocated the use of the CRF as a lipid predictor3-5 and has shown the superiority of the CRF as a lipid predictor.8 The ATD risk predicted by the CRF is graded with the lowest (minimal) risk afforded by a CRF of ≤0.59 and the highest risk by a CRF of ≥0.80. CRF values in the 0.70–0.79 range represent a high-risk category, though in a graded manner. CRF values in the 0.60– 0.69 range represent a lower risk category, though again in a graded manner. (These values are based on the precipitation method of HDL cholesterol measurement. If the enzymatic method is used, then the highest risk category is ≥0.70, the high- risk category is 0.60–0.69, the lower risk category, 0.50–0.59, and the minimal risk category is ≤0.49).
Treatment to stabilise/regress plaque in eight published angiographic regression trials depends on correction of hypertension and the dyslipidaemia risk factor.33 Using the CRF as the lipid arm and systolic blood pressure (SBP) as the barometric arm, a graph can be generated with the CRF on the ordinate and SBP on the abscissa. Additionally, a threshold line can be generated with CRF-SBP loci of (0.74,100) and (0.49,140) above which lies the CRF-SBP plots of 85% of the ATD patients in the author’s ATD database. (These co-ordinates are based on the precipitation method of HDL cholesterol measurement; if the enzymatic method is used, the co-ordinates are [0.62,100] and [0.40,140].) Any therapy that brings the patient’s CRF-SBP plot below the threshold line results in plaque stabilisation/regression in a minimum average of 75%.33 If LDL cholesterol goals are used instead, then any therapy that brings the LDL cholesterol level to <80 mg/dL (precipitation method of HDL cholesterol measurement but 70 mg/dL when the enzymatic method is used) results in stabilisation/regression of plaque in 93% of cases, and this is the case at any LDL cholesterol level below this threshold.34
The Program on the Surgical Control of the Hyperlipidemias (POSCH) was not structured to control blood pressure. As a result, significant plaque stabilisation/regression occurred in the face of marked hypertension. Consequently, at least in POSCH, plaque stabilisation/regression is purely a function of lipid changes. When LDL cholesterol levels are brought down to 99 mg/dL (2.5 mmol/L) or lower or when CRF levels are brought down to ≤0.59, plaque stabilisation/regression occurs in 99% of cases.35 Moreover, in POSCH, changes in the CRF perfectly predicted plaque outcomes. If the CRF rose at 1 year, then invariably angiographic plaque progressed at 3 years. If the CRF fell at 1 year, then invariably angiographic plaque stabilised/regressed at 3 years.35
Table 2 and Table 3 reveal that at any level of non-HDL cholesterol, a higher CRF portends an earlier age of ATD onset, while a lower CRF portends a later age of ATD onset in a linear fashion. The converse is not true: at any CRF value, a higher non-HDL cholesterol does not necessarily portend an earlier age of ATD onset and a lower non-HDL cholesterol does not necessarily portend a later age of ATD onset.
LDL cholesterol has long been the focus of interventional lipidologists for the prevention of primary or secondary ATD.36 The author has resurrected the Lipid Regulatory Hypothesis of Dr Esko Nikkila, and has shown that, at least in the POSCH37 and the National Heart Lung and Blood Institute (NHLBI) Type II Coronary Intervention Study,38 raising HDL cholesterol and lowering LDL cholesterol are both important in the stabilisation/regression of plaque.
One limitation of these findings is that they are based on a real-world observational study. During the study (4th November 1974–4th November 2003), full patient follow-up was not available. This is unfortunate, but unavoidable, in everyday practice of medicine in the USA. However, every case of ATD known to the author or reported to the author is reported here. The strengths of this study are that it represents the family practice of a single physician in a single location in a rural county with a relatively stable population over a long period of time. This study was undertaken at a time when lipid testing was not routinely done and the concept of treating dyslipidaemia was neither widely established nor accepted by either local patients or physicians.
Future directions of research involving non-HDL cholesterol should involve a broader look at all putative lipid predictors. The virtual reluctance of most investigators to use lipid ratios must be abandoned and lipid ratios given their place amongst the array of lipid predictors.
CONCLUSION
The concept of non-HDL cholesterol as a lipid predictor should be reconsidered due to the evidence of this study. While no randomised controlled clinical trial has been performed to validate the CRF, the outcomes of eight angiographic regression trials have been presented by the author. It would seem reasonable to dispense with non-HDL cholesterol and go back to the Framingham Heart Study concept of lipid ratios to determine the population at risk of ATD. The CRF is thus advocated as a lipid predictor worthy of note.








