BACKGROUND
Depression is a frequent comorbidity in patients with cardiovascular diseases, with a prevalence ranging from 35% to 74%.1-3 It is believed that the presence of a major depressive disorder may be an independent predictor of adverse cardiovascular outcomes.4 A possible explanation could be the dysregulated autonomic nervous system,5 leading to a higher incidence of malignant ventricular arrhythmias and, ultimately, sudden cardiac death.
The surface electrocardiogram can provide important information, with the heart rate-corrected QT interval being a non-invasive, easily accessible, and indirect measure of parasympathetic nervous system activity.6 With regards to the interplay between depressive disorders and QT interval, limited data are available in the existing literature to the authors’ knowledge.
MATERIALS AND METHODS
In the setting of the cross-sectional Corinthia study, the authors analysed participants aged 40 years or older who were not taking any QT-prolonging medication, such as antiarrhythmic drugs, antibiotics, antidepressants, or antipsychotics. The participants underwent clinical evaluation as well as self-assessment of depression through the Zung Self-Rating Depression Scale (SDS) for subjects below 65 years and the Geriatric Depression Scale (GDS) for older subjects. These two questionnaires were selected for their superior performance as self-rating scales. The presence of depression was considered in younger individuals with a Zung SDS score of ≥50 and in elderly with a GDS score of ≥5. Participants that did not complete the questionnaire were excluded from the analysis.
A resting 12-lead ECG with 10 sec duration was performed, with smart ECG measurement and interpretation programmes being used for automated measurement and interpretation of amplitudes and duration of ECG waves in each of the 12 leads. QT interval measurements were extracted from each individual lead after correction for heart rate (QTc) using Bazett’s formula. A QTc greater than 440 msec was defined as abnormal.
RESULTS
From the entire study population, 1,637 individuals (980 female and 657 male) were included in the final analysis. The younger age population with depression was predominantly female and had a higher prevalence of coronary artery disease. Interestingly, those classified as having depression had a longer QTc duration and percentage of abnormal QTc. No differences were noted in the other examined parameters. On the other hand, elderly individuals had similar values of QTc and percentage of abnormal QTc irrespective of depression status.
To test the impact of depression status on the duration of QTc interval, the authors performed a linear regression analysis according to age groups, adjusting for factors associated with QT prolongation. Importantly, the presence of depression was associated with increased QTc duration (by approximately 10.8 msec), independently from the confounders and only in the younger age subgroup. Similarly, depression was associated with approximately seven-fold higher prevalence of abnormal QTc in younger individuals, a finding that was not observed in the elderly participants (Figure 1).
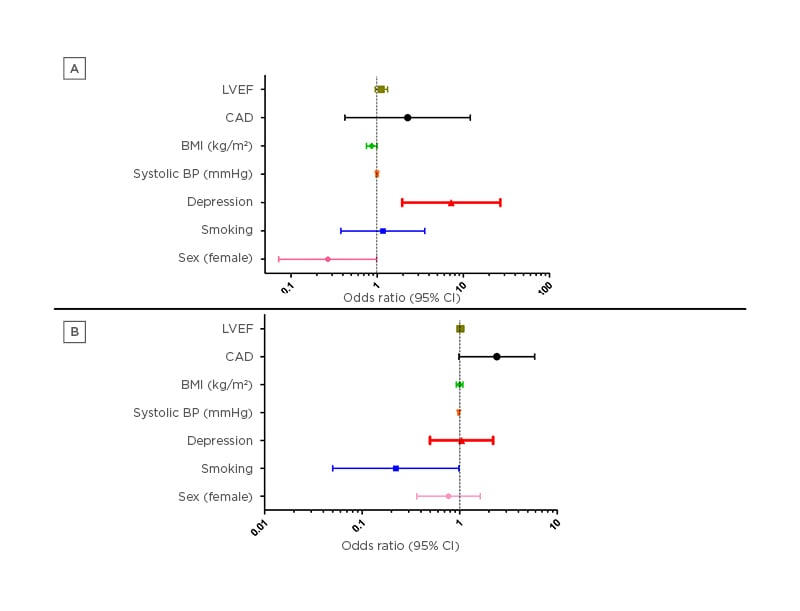
Figure 1: Logistic regression analysis concerning the impact of depression on abnormal corrected QT interval duration in A) younger and B) elderly individuals after adjustment for various factors implicated in QT prolongation.
BMI: body mass index; BP: blood pressure; CAD: coronary artery disease; CI: confidence interval; LVEF: left ventricular ejection fraction.
CONCLUSIONS
As the authors’ findings indicate, even though elderly individuals had increased QTc and a higher prevalence of abnormal QTc compared with younger participants, the presence of depression was associated with longer QTc only in the younger age subgroup, even after adjustment for known QT-prolonging factors. Moreover, the authors detected a greater prevalence of prolonged QTc in younger participants with depression, while in the elderly individuals no differences were noted concerning this parameter. The authors’ findings highlight the inter-relationship between emotional and cardiovascular health and the potential role of depression as a cardiovascular risk factor.








