BACKGROUND AND AIMS
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection has been associated with deregulations in vascular, endothelial, and myocardial function.1-7 Inflammation and oxidative stress have been suggested as possible pathophysiological mechanisms that lead to these impairments after COVID-19 infection.1-3 The aim of this study was to investigate premature alterations in arterial stiffness, in endothelial integrity, and in coronary and cardiac performance 4 months after COVID-19 infection.
MATERIALS AND METHODS
In this prospective observational case-control study, the authors consecutively recruited 70 patients 4 months after a confirmed infection by SARS-CoV-2, 70 age- and sex-matched patients with untreated hypertension (positive control), and 70 healthy individuals. The authors evaluated:
- perfused boundary region (PBR) of the sublingual arterial microvessels (increased PBR indicates reduced endothelial glycocalyx thickness);
- coronary flow reserve (CFR) by Doppler echocardiography;
- flow-mediated dilation (FMD);
- pulse wave velocity and central systolic blood pressure;
- left ventricular global longitudinal strain; and
- malondialdehyde (MDA), an oxidative stress marker.
RESULTS
Patients diagnosed with COVID-19 and patients with untreated hypertension displayed similar FMD and CFR, while both groups had lower FMD and CFR values than controls. Patients diagnosed with COVID-19 had similar PBR values with patients with untreated hypertension but both groups had greater PBR values compared to control group. Patients diagnosed with COVID-19 and patients with untreated hypertension had higher pulse wave velocity carotid-femoral and central aortic systolic blood pressure values compared with control group. Patients diagnosed with COVID-19 had similar left ventricular global longitudinal strain values with hypertensives but significantly different (less negative) from control group. Patients diagnosed with COVID-19 displayed much higher MDA levels than both patients with untreated hypertension and healthy individuals (Table 1).
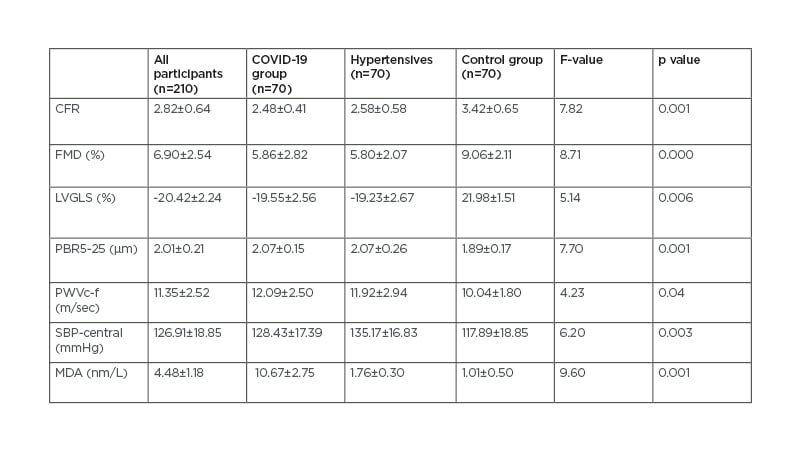
Table 1: Markers of cardiac and vascular function.
CFR: coronary flow reserve; FMD: flow mediated dilatation; LVGLS: left ventricular global longitudinal strain; MDA: malondialdehyde; PBR5-25: perfused boundary region of the sublingual vessels with diameter 5-25 μm; PWVc-f: pulse wave velocity carotid to femoral; SBP-central: central (aortic) systolic blood pressure.
CONCLUSION
SARS-CoV-2 infection may cause endothelial and vascular dysfunction, which are linked to impaired longitudinal myocardial deformation 4 months after COVID-19 infection. The 10-fold increase of MDA in patients diagnosed with COVID-19 relative to patients with untreated hypertension and normal control indicate oxidative stress as a possible pathophysiological mechanism contributing to vascular, endothelial, and myocardial deregulations.








