BACKGROUND AND AIMS
Globally, cardiovascular diseases remain the leading cause of death, taking an estimated 17.9 million lives each year. It is projected that the global burden of cardiovascular diseases will continue to rise.1,2 The majority of patients with cardiovascular diseases have a significant symptom burden with comorbidities, and often have a progressive course towards end-stage disease and, ultimately, death.2 For this reason, early integration of palliative care into the care of cardiovascular patients is recommended.3,4 However, palliative care has not yet become an integral part of care for patients with cardiovascular diseases, as only a small proportion of patients are referred for palliative care consultations. Furthermore, referral often occurs too late in the disease course.2,5,6 In order to improve the rate of referral to palliative care by cardiologists, there is a need to scrutinise current referral practices to palliative care from the cardiology department. Therefore, the present study aimed to examine the time between referral to palliative care and death; the clinical profile of patients referred; and the place of death of patients with cardiovascular diseases who were referred to palliative care from the cardiology department, using data from 2010–2020.
MATERIALS AND METHODS
This retrospective descriptive study included all patients who were referred to the Mobile Palliative Care Team from the cardiology unit in the large University Hospital Besançon, France, between 2010–2020. The following information was extracted from the medical hospital files: date of first referral to the palliative care team; vital status (alive/dead) at the study cut-off date (31st December 2020); sex; date of birth; main underlying disease; the motive for hospitalisation at the time the palliative care team was contacted; and for patients who died, their date of death, cause of death, and place of death.
RESULTS
Of the 142 included patients, 134 (94%) died, and 8 (6%) were still alive as of July 2022. The mean age at the time of death was 75±14 years. The median time between referral to palliative care and death was 9 days (first quartile, third quartile: 2, 37.5; range: 0–5.8 years). The number of referrals from the cardiology department per year did not increase over time. As the main life-limiting disease, most patients had chronic heart failure (54%), followed by other cardiovascular diseases (valve, acute coronary syndrome, congenital, or stroke [20%]), and cancer (14%). The main motives for hospitalisation at the time the palliative care team was contacted were acute decompensation of heart failure (72%), acute coronary syndrome (11%), and infective endocarditis or pulmonary embolism (9%). The place of death was available for 118 patients (Figure 1). The majority of patients (n=73; 54%) died in the cardiology department of University Hospital Besançon, 14 patients (10%) died in the palliative care unit, and only 17 patients (13%) died at home.
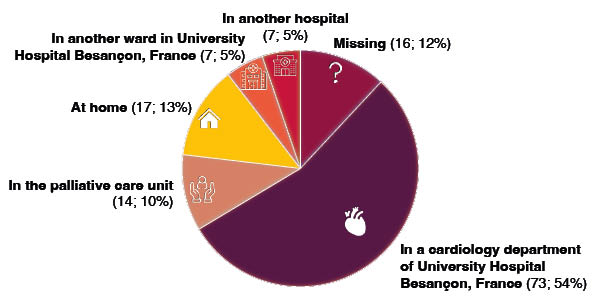
Figure 1: Visual representation of the places of death of patients with cardiovascular disease who were referred to the mobile palliative care team (n=134).
CONCLUSION
This study showed that referral of patients to palliative care from the cardiology department is suboptimal, as the referral is often only initiated very close to the time of death. In addition, a large proportion of patients still die in the hospital setting. It is noteworthy that palliative care is mainly provided to paitents with heart failure after acute decompensation. Further prospective studies are warranted to investigate whether these dispositions correspond to patients’ wishes and end-of-life care needs, and future studies should investigate how the integration of palliative care into the care of patients with cardiovascular diseases can be improved.








