BACKGROUND
Antithrombotic therapy in transcatheter aortic valve replacement (TAVR) is highly controversial. Dual antiplatelet therapy (DAPT) for 3–6 months with aspirin and clopidogrel is the current recommendation. In patients with an indication for oral anticoagulation (OAC), several regimes were described, ranging from OAC monotherapy, to dual, and even triple therapy. Besides vitamin K antagonists, non-vitamin K OAC (NOAC) are frequently used in TAVR patients with an indication for permanent OAC.
PURPOSE
The authors aimed to evaluate different antithrombotic regimes and their impact on the outcome.
METHODS
A single-centre retrospective analysis was performed in 1,160 patients treated by transfemoral TAVR approach (TF-TAVR).1 Primary endpoints were 30-day mortality, stroke, and bleeding according to VARC-2 criteria. The secondary endpoint was all-cause mortality at 1 year.
RESULTS
In 1,160 patients with TF-TAVR, a broad range of regimes occurred in clinical practice. The majority of patients were on DAPT (637 patients; 55%), followed by vitamin K antagonists + clopidogrel (186 patients; 16%). Other patients received OAC mono (98 patients; 9%), triple therapy (93 patients; 8%), NOAC mono (31 patients; 3%), single antiplatelet therapy (SAPT [40 patients; 4%]) or NOAC + clopidogrel (31 patients; 3%).
All-cause mortality 30 days after TF-TAVR differed between the regimens (SAPT/OAC+SAPT/N-OAC+DAPT: 0.0% versus DAPT: 3.6% versus OAC: 10.2% versus NOAC: 1.3% versus NOAC+SAPT: 0.3%; pANOVA <0.0001). Severe bleeding events were comparable (SAPT: 5.0% versus DAPT: 2.4% versus OAC: 7.1% versus NOAC: 1.3% versus OAC+SAPT: 3.2% versus NOAC+SAPT: 0.0% versus N-OAC+SDPT: 4.3%; pANOVA=0.15). Stroke rates were comparable in all subcohorts as well (SAPT: 5.0% versus DAPT: 3.0% versus OAC: 7.1% versus NOAC: 2.7% versus OAC+SAPT: 1.6% versus NOAC+SAPT: 0.0% versus N-OAC+DAPT: 1.1%; pANOVA=0.13). Only two haemorrhagic strokes (5.6%) appeared under DAPT and OAC mono respectively, whereas all others were of thromboembolic origin (94.4%).Surprisingly, all-cause mortality at 1 year after TF-TAVR was higher in OAC patients compared to all other used regimes (log rank overall: p=0.0012).
CONCLUSION
Data from this retrospective analysis indicate that a variety of different antithrombotic regimes occur even in a single centre analysis. All-cause mortality was enhanced in patients with OAC. Therefore, clinical trials need to investigate if this can only be explained by additional atrial fibrillation.
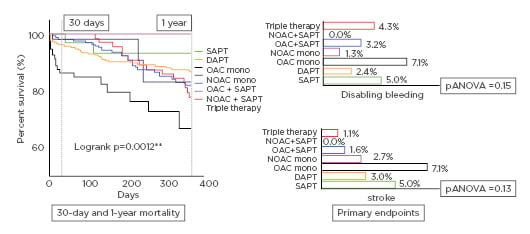
Figure 1: Primary and secondary endpoints.
DAPT: dual antiplatelet therapy; OAC: oral anticoagulation; NOAC: nonvitamin K oral anticoagulation; SAPT: single antiplatelet therapy.








