Abstract
Atrial fibrillation (AF), the most common form of arrhythmia, is fast becoming one of the world’s most significant health issues. It is well established that AF increases the risk of mortality, and is associated with significant morbidity, including an increased risk of stroke. AF also worsens quality of life for patients, which can also be a burden for caregivers. As a result of Europe’s ageing population, the prevalence of AF is expected to rise substantially in the future. With more patients expected to be affected by AF, rates for AF-related strokes, hospitalisations, and doctor visits are also expected to rise, ultimately raising healthcare system costs across Europe. It is estimated that up to 2.6% of total annual healthcare expenditure is associated with AF in European countries. The high cost of AF is largely attributable to hospitalisations and complications such as stroke, i.e., in 2015, stroke was estimated to cost €45 billion a year in the European Union (EU). The purpose of this review is to highlight the current scale and growing burden of this new millennium epidemic in Europe. This review aims to foster a greater awareness and understanding of the magnitude of the clinical, patient, and economic burden of AF. An understanding of the burden of AF is imperative for directing care pathway management and healthcare policies that can help alleviate the burden of AF experienced by patients, caregivers, and healthcare systems in Europe.
INTRODUCTION
Atrial fibrillation (AF), the most common form of arrhythmia, is characterised by an irregular and often fast heart rhythm resulting in uncoordinated contraction of the atria. Patients with AF have an increased risk of life-threatening complications and other diseases, and AF also increases the risk for heart failure 5.0-fold, stroke 2.4-fold, and mortality 2.0-fold.1 Furthermore, AF worsens quality of life (QoL) for patients and caregivers,2-7 increasingly places a critical financial burden on healthcare systems, and is rapidly becoming one of the world’s most significant health issues.
Currently, >11 million patients are estimated to have AF in Europe,8 and the total healthcare costs of AF account for ≤2.6% of total healthcare expenditure in Europe.9-12 Due to Europe’s growing population, the prevalence of AF is expected to rise substantially with more patients expected to be affected by AF in the future. Rates for AF-related strokes, hospitalisations, and doctor visits are also expected to increase, ultimately raising the cost of healthcare systems across Europe. On account of the profound impact AF is expected to have in Europe, the magnitude of the clinical and economic burden of AF must be further investigated to help direct care pathway management and healthcare policies that can be used to alleviate this burden among patients, caregivers, and healthcare systems. The objective of this review is to raise awareness and understanding of the burden of AF in Europe, with a focus on France, Germany, Italy, and the UK.
EPIDEMIOLOGY OF ATRIAL FIBRILLATION
AF is categorised into several types. Patients are categorised on their most frequent pattern of AF and may have episodes of AF that fall into one or more of the following categories: paroxysmal (occasional AF that stops ≤7 days), early persistent (AF that lasts 7 days to 3 months), persistent (continuous AF for >7 days), long-standing persistent (episodes occur for >12 months), or permanent (episodes continue and attempts to restore sinus rhythm are ceased).13,14 In Europe, 75% of patients with AF have paroxysmal or persistent AF.15
Demographics, Causes, and Risk Factors of Atrial Fibrillation
AF is a common age-related arrhythmia, affecting 1 in 4 adults ≥40 years of age during their lifetime;16 furthermore, nearly 8 in 10 adults with AF are ≥65 years of age8 and the condition occurs more frequently in males than females.8 Specifically, among adults of European descent ≥40 years of age, men are 13% more likely to develop AF than women during their lifetime.16 As many as 1 in 4 patients are diagnosed with AF after suffering a stroke.14
AF develops from structural changes to the heart due to lifestyle, other chronic conditions, and nonmodifiable factors. Abnormalities or damage to the heart’s structure are the most common cause of AF, and this can be the result of high blood pressure, heart attacks, coronary artery disease, abnormal heart valves, congenital heart defects, previous heart surgery, sick sinus syndrome, an overactive thyroid or other metabolic imbalance, sleep apnoea, lung diseases, or stress due to pneumonia, surgery, or other illnesses.13,14,16 Other factors can also cause AF, including exposure to stimulants, such as medications, caffeine, tobacco, or alcohol; lifestyle factors, including obesity17,18 and alcohol consumption;14,17 risks of cardiovascular disease, including smoking, stress, caffeine, and other stimulants;14 and activity level.13,14,17 Additional conditions e.g., high blood pressure,17 heart failure,16,19 history of heart attack,16 coronary artery and other heart disease,16,18 previous surgery,20 sleep-disordered breathing (e.g., obstructive sleep apnoea),17 and diabetes17,21 also increase the risk of developing AF. Furthermore, nonmodifiable factors including older age,14,22 congenital heart defects,23 family history or other genetic factors,16,24 and male sex14,22 also add to the risk of developing AF.
The Current Scale and Growing Future Prevalence and Incidence of Atrial Fibrillation in Europe
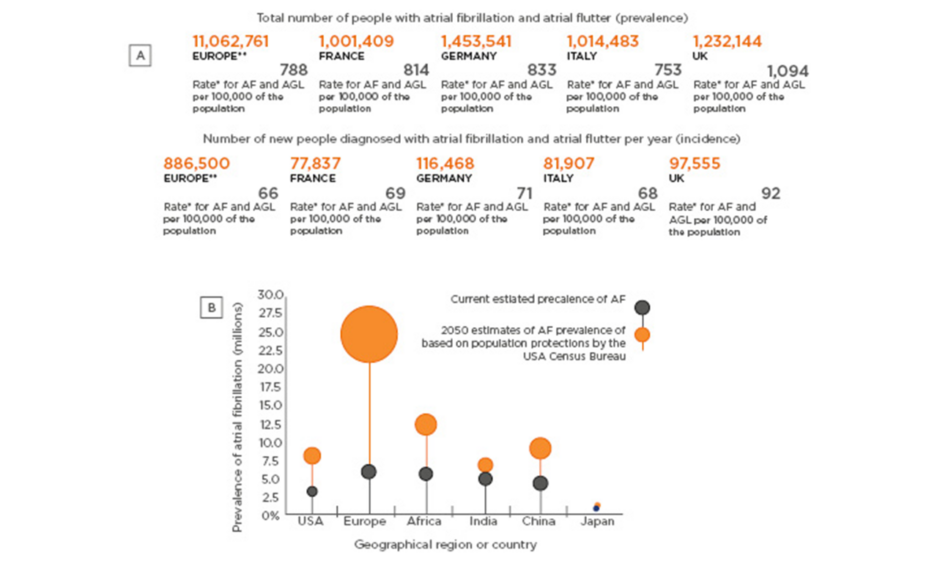
AF is the most common type of cardiac arrhythmia worldwide, affecting >5.5 million people in the USA,25 >16 million people across Asia Pacific,26 and >11 million people in Europe (Figure 1A).8,27 Over 1 million people are afflicted by AF in each of France, Germany, Italy, and the UK.8 The number of new people diagnosed each year with AF in Europe is >886,000, but incidence rates vary by region, from nearly 78,000 in France to >116,000 in Germany (Figure 1A).8 AF is almost as common as stroke and cancer within Europe, including in France, Germany, Italy, and the UK.8
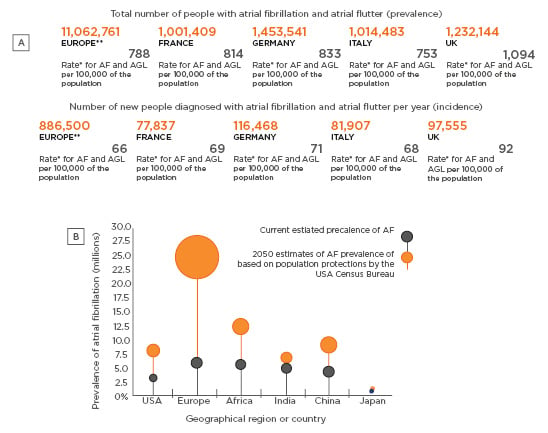
Figure 1: Prevalence and incidence of atrial fibrillation and 2050 estimated prevalence of atrial fibrillation in Europe compared to other geographical regions or countries.
A: Prevalence and incidence of atrial fibrillation (AF) and atrial flutter in Europe. *Age-standardised values. **Obtained for Europe, part of the Four World Regions category in the online Global Burden of Disease tool. Adapted from Global Burden of Disease Collaborative Network (2016).27 B: Current estimated prevalence of AF and 2050 estimated prevalence of AF. Adapted from Rahman et al. (2014).29 AF: atrial fibrillation; AFL: atrial flutter.
European countries have ageing populations that are growing rapidly,28 and estimates suggest that over the next 11 years, there will be a 70% increase in the number of people affected by AF in Europe (the prevalence and incidence estimates of AF in Europe combine rates for AF and atrial flutter).19 By 2050, Europe is projected to have the greatest increase in AF compared to other regions globally (Figure 1B).29 With the growing number of patients affected by AF in Europe, the number of AF-related stroke events and medical visits are also expected to increase within the next 11 years by an additional 280–340,000 new ischaemic strokes, 3.5–4 million hospitalisations for AF, and 100–220 million outpatient visits.19
CLINICAL BURDEN OF ATRIAL FIBRILLATION
Symptoms of Atrial Fibrillation
AF and its related symptoms are a major therapeutic challenge and burden to healthcare systems.30 The symptoms of AF disrupt daily life and range from mild to debilitating.5 The frequency and severity of symptoms varies from patient to patient, and within a patient, and symptoms can fluctuate widely over time. These factors contribute to challenges in clinical decision-making in management of treatment.30 The most common symptoms are palpitations (65%), fatigue (50%), shortness of breath (43%), malaise (30%), dizziness (19%), anxiety (12%), chest pain (12%), and other symptoms (5%),19,30,31 and >50% of AF patients have a reduced ability to exercise.30
An estimated 15–30% of AF patients experience silent AF, meaning that their AF is not associated with symptoms.30 Asymptomatic AF patients may be at a greater risk of complications and disease severity due to lack of treatment. Patients with silent AF experience a decreased general health and QoL compared to healthy individuals, which is driven by their comorbid conditions.32 The pattern of AF is different among symptomatic and asymptomatic patients, i.e., persistent and permanent AF are two and three times more common in asymptomatic patients than symptomatic patients, respectively.15 The higher pattern of permanent AF among asymptomatic AF patients than in symptomatic patients is primarily due to lower treatment management, given its asymptomatic nature.15
Clinical Consequences of Atrial Fibrillation
AF increases a patient’s risk of life-threatening events and conditions, including stroke, heart failure, and death. Compared to patients without AF, AF patients have an increased relative risk of heart failure (399%), major cardiovascular events (96%), ischaemic heart disease (61%), chronic kidney disease (64%), dementia or cognitive impairment (40%), peripheral artery disease (31%), and cardiovascular mortality (103%).1,17,33 Stroke is a serious complication of AF that is associated with long-term disability and mortality. Based on pooled estimates from studies conducted in the last 5 years, patients with AF have a 142% increased risk of any stroke and a 133% increased risk of ischaemic stroke.1 Stroke in AF patients is more severe and debilitating than in patients who do not have AF. Analysis of the North Dublin Population Stroke Study revealed that patients with AF have greater neurologic impairment and functional disability than patients without AF, and ≤3 months after a stroke, patients with AF are significantly more disabled than patients without AF.34 In general, an estimated 30% of stroke patients will have a second stroke, and risk of a second stroke is nearly 9-fold higher than that in the general population.35 Heart failure is a common complication of AF that increases the risk of mortality and lengthens hospital stay.36,37 The risk of mortality is two times greater in heart failure patients with a new AF diagnosis, than in heart failure patients without AF.19 Furthermore, AF is independently associated with a significantly greater risk of mortality even without the presence of other conditions; patients with AF have a 46% greater risk of mortality than patients without AF, based on pooled estimates from studies in the last 5 years.1,17
Impact on Quality of Life
Patients with AF have a significantly lower QoL than the general population as measured byvarious validated QoL instruments.3-5,7,38 The symptoms experienced by patients with AF have been associated with a 19% impairment in functional status, based on functional capacity as measured by the Goldman Specific Activity Scale,38 a 25% disruption to daily activities as measured using the illness intrusiveness scale,39 and a ≤47% reduction in QoL as measured using the SF-36 QoL scale.38,39 Patients with AF or other cardiovascular diseases such as coronary artery disease, congestive heart failure, and history of heart attack have similar reductions in QoL.7,38 Patients with intermittent AF, paroxysmal, and early persistent AF, have worse QoL than those with chronic AF (persistent and permanent AF).5
Severe consequences of AF, such as stroke, can have a devastating impact on patient QoL and the ability to perform daily activities. Stroke can cause significant impairment in physical, psychological, and social function, and can reduce a patient’s ability to carry out routine activities.40 Limitations a patient might experience after a stroke include paralysis, depression, personality changes, problems with communication, anxiety, memory loss, and cognitive impairment.40 Furthermore, AF-related stroke is more severe and more devastating than stroke in patients who do not have AF.34,41
Burden of Atrial Fibrillation to Caregivers
Caring for family members with AF can be burdensome. Some form of caregiver assistance is required in 63% of elderly patients with AF,42 and in 80% of AF patients recovering from stroke.6 Patients with AF may require caregiver assistance for many activities associated with daily living. These include assisting with activities that the individual struggles with due to tiredness; assisting or confirming correct dosage of medication and administration of medication; monitoring for signs of bleeding; providing assistance and transportation to medical appointments, including with the primary care physician or anticoagulation clinic for regular monitoring; and/or ensuring adherence to any dietary restrictions.43 As a result, caregivers of patients with AF experience considerable changes to their daily lives, including potential disruptions to their schedules, lack of family support, health problems, and financial burden.2 Caregivers are at high risk of burnout when they are required to provide care for long hours and when they care for patients who are frail, sick, or disabled; for those patients who have low QoL; have experienced or are at high risk of stroke; and patients with low levels of independence.2,6 Burden to caregivers may in turn lead to inadequate patient support, physical and emotional stress, caregiver burnout, andsuboptimal patient care outcomes.43
ECONOMIC BURDEN OF ATRIAL FIBRILLATION
Total Healthcare Costs
The economic burden of AF is high and places a critical financial burden on healthcare systems in Europe. The reported annual healthcare costs of AF range from €660–3,286 million (France: €1,942 million,11 Germany: €660 million,10,44 Italy: €3,286,10 and the UK: £1,30712), accounting for 0.28–2.60% (France: 2.60%,11 Germany: 0.28%,10,44 Italy: 2.49,10 and the UK: 0.90–2.4%12) of total healthcare spending (Figure 2A). It is important to note that the cost associated with AF and the percentage of total healthcare spending for France is based on in-patient and rehabilitation costs to hospitals for AF patients hospitalised for cardiovascular reasons only (excluded in the study were minor cardiovascular complications, community consultation, and prescription); therefore, these costs likely do not fully represent the total cost in France.11Moreover, estimates for Germany10,44 and the UK12 are based on direct costs only. The high cost of AF is largely attributable to hospitalisations and complications such as stroke.10,12 National healthcare costs for AF in these countries are similar to those for other cardiovascular diseases (e.g., heart failure, stroke, coronary artery disease, angina, and acute coronary syndrome).11,12,44-49 Although the costing studies were conducted across different timespans and measure different variations of cost, the high cost burden AF places on healthcare systems in Europe is unequivocal.
Direct and Indirect Costs
Direct (e.g., hospitalisations, outpatient and physician visits, prescriptions, laboratory testing, and long-term care) and indirect (e.g., work productivity losses and support provided by caregivers) costs for the management of AF are highly variable across European countries.Direct costs are high, and account for 2.6% of hospital expenditures in France11 and 0.9–2.4% of total annual healthcare expenditures in the UK.12 Annual direct per-patient costs are similar in France,50 Germany,51,52 Italy,53 and the UK,12 and annual indirect per-patient costs are highly variable by country, with the highest costs reported in Germany49,51,53 (Figure 2B).
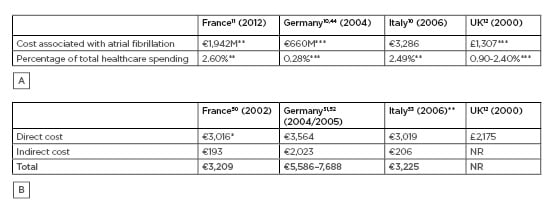
Figure 2: Healthcare costs of atrial fibrillation in France, Germany, Italy, and the UK.
A: Annual total healthcare costs of atrial fibrillation (AF). *Based on limited country data reporting. **Based on inpatient and rehabilitation costs to hospitals for AF patients hospitalised for cardiovascular reasons (study excluded minor cardiovascular complications, community consultation, and prescription; therefore, these costs do not represent the total cost in France). ***Based on direct costs. B: Annual direct and indirect cost of AF per patient. Direct cost was calculated by excluding costs for loss of work from the total per-patient cost reported for the societal perspective in Le Heuzey et al.21 Drug costs contained out-of-pocket costs; however, the authors noted that these costs were not statistically different from the those in the healthcare payer perspective; therefore, drug costs were assumed to be direct costs. **Based on 1-year follow-up costs after index admission. AF: atrial fibrillation; NR: not reported.
Persistent AF can cost significantly more to treat than paroxysmal or permanent AF. In one analysis of direct and indirect costs in patients with AF in Germany and Sweden, costs were lowest for permanent AF and highest for persistent AF in Germany; however, in Sweden costs were equally high for paroxysmal and persistent AF.50 Lower costs for permanent AF can be attributed to the fact that the presence of AF is accepted by the patient and the physician, and a decision has been made not to pursue treatment to restore or maintain sinus rhythm.13,14
Hospital costs represent the largest expense in AF management, and account for 44–78% of AF management costs.10,12,44,51,53 In-patient costs account for 50–70% of annual direct costs.9 The reported mean annual cost of in-patient care per patient in Europe is variable, with the highest costs reported in France and Germany (in-patient cost: France: €3,016,21 Germany: €2,464–6,000,50,51 Italy: €1,778,53 and the UK: £1,67912). Healthcare resource use in AF patients is high, with ≤40% of AF patients hospitalised each year primarily due to heart failure and arrhythmia recurrence.14 Hospitalisation costs can be two times higher for persistent AF than paroxysmal AF,21 and other factors associated with a high hospital cost include stroke and bleeding events, high stroke risk, high bleeding risk, and presence of other conditions.54
The Impact of Stroke on the Costs of Atrial Fibrillation
The cost for the treatment and prevention of stroke in AF is high, contributing substantially to the total healthcare cost of AF. In Europe, the cost of AF-related stroke is 7–60% higher than the cost of stroke in patients without AF.11,41,55-60 Higher costs associated with AF-related stroke are due to hospitalisations, inpatient rehabilitation, longer hospital stays, hospital readmissions, and greater use of nursing care.9,55 In 2015, stroke was estimated to cost €45 billion a year in the European Union (EU).61 Contributing to this burden were direct healthcare costs (€20 billion), informal care (€16 billion), and productivity losses (€9 billion).61 The annual per-patient costs for AF-related stroke for France,11 Germany,55 Italy,62 and the UK56 are presented in Figure 3. Although the studies are from different years, ranging from 2002 to 2015, and measure different variations of cost, it is clear that the annual per-patient cost of stroke across these European countries is substantial.
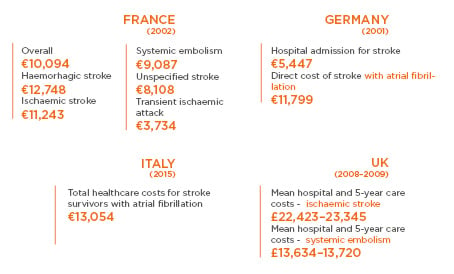
Figure 3: Annual per-patient cost of atrial fibrillation-related stroke in France,11 Germany,55 Italy,62 and the UK.56
FUTURE DIRECTIONS
Although this review provides a comprehensive summary of the burden of AF in Europe based on the available literature, the epidemiological, clinical, and economic findings are mostly based on a limited number of studies that were published over the past 10 years. Because diagnostic and management strategies for AF have evolved and changed dramatically from the previous decade, it is conceivable that the results presented in this review may overestimate or underestimate the true economic burden of AF. More recent studies are needed to further elucidate the current burden of AF for Europe and individual European countries. The 2016 European Society of Cardiology’s (ESC) guidelines for the Management of AF also highlights several gaps in the knowledge, where evidence is currently being developed or requires additional research, which will help to further establish the magnitude of the burden of AF.14 In particular, the guidelines suggest that several specific AF groups should be studied to better characterise their risk of AF, stroke, and other AF-related comorbidities e.g., patients with one stroke risk factor, non-Caucasian patients, and female patients. Differences in the overall management e.g., different treatment for concomitant cardiovascular diseases, may help explain the variability in the reported rates of new (incident) AF cases, all (prevalent) AF cases, and AF complications. The guidelines also highlight that the major causes of AF require better characterisation by patient group, and should consider the key comorbidities associated with AF and pathophysiological distinct types of AF.14 In addition, the guidelines suggest that models of care that integrate patient shared-decision- making to identify appropriate care pathway management may be of particular value in the management of AF. Further research is needed to identify the number of patients affected by AF, the impact on disease progression, and the management costs among different patient subgroups.
CONCLUSIONS
This review promotes a greater awareness and understanding of the magnitude of the clinical, patient, and economic burden of AF to caregivers and healthcare systems in Europe. AF affects an estimated 11 million people in Europe and by 2050, Europe is projected to have the greatest increase in AF (to 18 million people) compared to other regions globally. Patients with AF have an increased risk of mortality and comorbidities, such as risk of heart failure, as well as significant decreases in QoL which can be burdensome to their caregivers. The reported annual healthcare costs of AF in France, Germany, Italy, and the UK ranges from €660–3,286 million, accounting for 0.28–2.60% of total healthcare spending in these European countries. The high cost of AF is largely attributable to hospitalisations and complications such as stroke. In 2015, stroke was estimated to cost €45 billion a year in the EU. Ongoing and future epidemiological, clinical, and costing studies are necessary to understand the full scale of the clinical, patient, and cost burden of AF for Europe and individual European counties. The data gathered thus far warrants greater need and attention in understanding and tackling this new millennium epidemic.