Abstract
In this review, two cases of severe pulmonary hypertension of different classes that have been successfully treated using inhaled nitroglycerine are presented. In a community hospital setting and in cases of life-threatening right heart failure and shock not responding to simple traditional treatments, thought should be given to the use of inhaled nitroglycerine. Inhaled nitroglycerine is practical, cheap, and readily available in any hospital without reconstitution. This approach may allow for the treatment, or at least temporary stabilisation, of these patients until transferred to a tertiary care facility.
INTRODUCTION
Pulmonary hypertension as a cause of right-sided heart failure and shock is often missed. In the intensive care patient population, there are multiple causes of acute on chronic elevation of pulmonary artery pressure. These causes include, but are not limited to, hypoxia, hypercarbia, left ventricular ischaemia or infarction, hypothermia, hyperviscosity, supine position, positive pressure ventilation, high positive end expiratory pressure, and lung parenchymal inflammation as a result of acute lung injury or acute respiratory distress syndrome. Therefore, diagnosis of acute cor pulmonale requires a high degree of suspicion, particularly if shock is not responding to the usual treatment modalities.
Inhaled nitric oxide is a fairly well established method used for the acute and temporary reduction of pulmonary artery pressure.1 Inhaled nitric oxide has also been established in primary pulmonary hypertension in predicting which patients might respond to phosphodiesterase inhibitors or calcium channel blockers.2-7 A prospective study of 14 adult patients with pulmonary hypertension after cardiac surgery demonstrated selective pulmonary vascular dilatation and selective decrease in pulmonary vascular resistance when using inhaled nitric oxide as opposed to intravenous nitroglycerine and intravenous prostaglandin E1.8 The study failed to demonstrate improvement in cardiac output and right ventricular ejection fraction when the starting right ventricular function was not compromised. The study also demonstrated significant elevation of median methaemoglobin concentration when nitric oxide was used.
When given intravenously, nitroglycerine breaks down into nitric oxide and thus is considered a nitric oxide donor, and provides an explanation for the short duration of action. Nitroglycerine is a potent venodilator. A small animal study showed that inhaled nitroglycerine is superior to intravenous nitroglycerine in improving pulmonary hypertension and haemodynamics, and decreasing shunting.9 Inhaled nitroglycerine has been studied in pulmonary hypertension Class 1 children with acrocyanotic congenital heart disease. It showed a reduction in pulmonary arterial pressures and pulmonary vascular resistance without any effect in systemic arterial pressures.10 The authors propose that the mechanism of action of inhaled nitroglycerine is a break-down into nitric oxide in the pulmonary vascular bed adjacent to ventilated alveoli resulting in pulmonary venodilation and reduction in pulmonary arterial pressure and vascular resistance.
To the authors’ knowledge, the literature for use of inhaled nitroglycerine is limited to the paediatric and surgical settings and have not been evaluated in adult patients in the intensive care unit. Here, two cases of pulmonary hypertension and impending acute right ventricular failure that were treated with inhaled nitroglycerine and had favourable outcomes are presented. This treatment could be used as an alternative to more expensive inhaled medications such as inhaled nitric oxide and inhaled iloprost.
CASE REPORT
Patient 1
A 23-year-old female with a past medical history of asthma and severe scoliosis resulting in acute long-standing pulmonary hypertension presented to the intensive care unit. The patient was not compliant with home O2. She also had a history of pulmonary embolism 18 months prior, for which she received 6 months of anticoagulants. The patient was admitted to the intensive care unit for increased work of breathing, hypoxia, community-acquired pneumonia, and possible asthma exacerbation. She was started on ceftriaxone, azithromycin, methylprednisolone, and a salbutamol nebuliser. She had an initial improvement; however, late the next day she developed increased work of breathing and was intubated and mechanically ventilated for hypoxic respiratory failure. Although she continued to be afebrile her antibiotic spectrum was expanded empirically.
A transthoracic echocardiogram (ECG) obtained on the following day demonstrated normal ventricular function with severe pulmonary hypertension and dilated right atrium. A pulmonary artery catheter was placed to further define her pulmonary hypertension. Haemodynamic parameters included elevated pulmonary pressures measuring 105/75 mmHg.
The patient was given sildenafil 20 mg enterally three times daily, amlodipine besylate 5 mg enterally daily, and inhaled nitroglycerin nebuliser at a rate of 1.7 mg/hour (concentration 200 µg/mL nebulised at 6 L/min O2 flow using large volume nebuliser).
There was a dramatic reduction in pulmonary arterial pressures to 50% of baseline within 6 hours while the systemic vascular resistance and systemic blood pressure remained stable (Table 1).
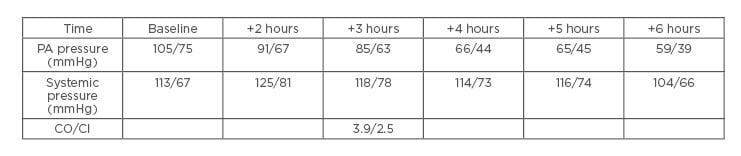
Table 1: Haemodynamic parameters in the first 6 hours after pulmonary artery catheter placement. Inhaled nitroglycerin nebuliser was started at +1 hours.
CI: cardiac index; CO: cardiac output; PA: pulmonary arterial.
The patient was then transferred to a tertiary care centre for long-term management of her pulmonary hypertension where she was transitioned to inhaled iloprost. Ultimately, she failed to be liberated from mechanical ventilation. A tracheostomy was performed, and she was discharged to a rehabilitation centre for long-term ventilator weaning.
Patient 2
A 77-year-old female presented to the intensive care unit from a rehab facility with severe dyspnoea and a change of mental status. The patient had a past medical history significant of atrial fibrillation, congestive heart failure with an ejection fraction of 60%, chronic obstructive pulmonary disease, dyslipidaemia, and multiple myeloma. The patient presented with congestive heart failure which deteriorated in cardiogenic shock, respiratory failure, and anuria.
Her arterial blood gas showed a pH of 7.18, partial pressure of CO2 of 103 mmHg and partial pressure of O2 of 77 mmHg on 100% rebreather mask, a brain natriuretic peptide level of 1180 pg/mL, a serum sodium of 145 milliequivalents/L, potassium of 5.5 milliequivalents/L, blood urea nitrogen of 46 mg/dL, creatinine of 1.8 mg/dL, and troponin of 2.2 µg/L. Chest radiograph showed pulmonary vascular congestion with possible right middle and lower lobe infiltrates and right-sided moderate sized pleural effusion. ECG showed atrial fibrillation, heart rate of 82, and non-specific T wave, ST segment abnormalities.
Transthoracic ECG revealed an ejection fraction of 20%, global left ventricular hypokinesis, significant mitral valve thickening, mitral annular calcification, moderate-to-severe mitral stenosis with an estimated valve area of 1.5 cm2, moderate-to-severe mitral regurgitation, and estimated pulmonary arterial systolic pressure of 65 mmHg.
The patient was intubated and mechanically ventilated. She received broad spectrum antibiotics, dobutamine infusion, digoxin, sildenafil, and furosemide infusion during different times of the intensive care unit stay with no improvement.
Five days later, a repeat ECG showed an ejection fraction of 40% on dobutamine and an estimated pulmonary artery systolic pressure of 100 mmHg. A pulmonary artery catheter was placed. The haemodynamic numbers were a cardiac output of 5 L/min, cardiac index of 3 L/min/m2, stroke volume of 52 mL, central venous pressure of 21, systemic vascular resistance of 1,599 dynes/sec·cm5, pulmonary artery pressure of 94/28. Pulmonary capillary wedge pressure was unobtainable (Table 2).
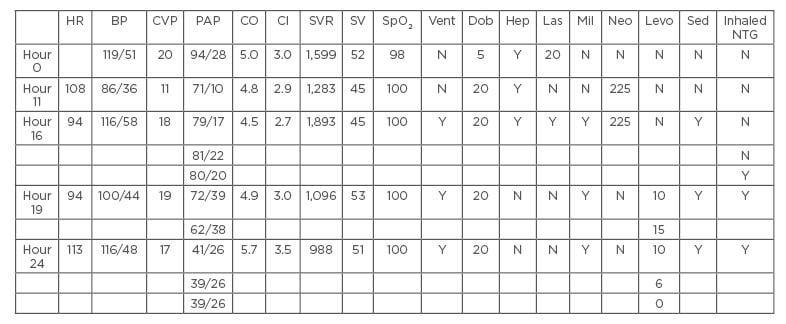
Table 2: Haemodynamic parameters starting from the time pulmonary artery catheter was inserted.
BP: blood pressure; CI: cardiac index; CO: cardiac output; CVP: central venous pressure; Dob: dobutamine; Hep: heparin; HR: heart rate; inhaled NTG: inhaled nitroglycerine; Las: furosemide infusion; Levo: noradrenaline; Mil: milrinone; N: no; Neo: neo-synephrine; PAP: pulmonary arterial pressure; Sed: sedation; SpO2: oxygen saturation; SV: stroke volume; SVR: systemic vascular resistance; Vent: ventilator; Y: yes.
Inhaled nitroglycerine was started at a concentration of 200 µg/mL and the patient was nebulised using large volume nebuliser set at an O2 delivery rate of 6 L/min. That resulted in the delivery of approximately 17 M (3.4 mg nitroglycerine) every 2 hours. Dramatic rapid reduction in pulmonary arterial pressure was noted with a decrease in pressor requirements. Approximately 12 hours later, the patient was completely weaned off noradrenaline. The patient was transferred to tertiary care centre for chronic management of pulmonary hypertension. Blood pressure was stable even after stopping inhaled nitroglycerine.
The patient was stabilised sufficiently for transfer to a tertiary care centre. Four days later the patient had persistent renal failure that required dialysis. During the insertion of femoral dialysis catheter, the patient developed a large retroperitoneal haematoma and unfortunately died from haemorrhagic shock.
DISCUSSION
Here, two cases of pulmonary hypertension and acute right heart failure that responded favourably to inhaled nitroglycerine are reported. The first case had pulmonary hypertension in Group III of World Health Organization (WHO) classification (pulmonary hypertension with hypoxaemia).11 Her severely elevated pulmonary pressures and acute right heart syndrome were likely as a result of an acute infection superimposed on chronic cor pulmonale. The authors speculate that her significant acute improvement in pulmonary haemodynamics with nebulised nitroglycerine, coupled with improvement in her oxygenation, was due to preferential vasodilation of pulmonary capillaries exchanging with ventilated areas alveolar units. The reduction of the pulmonary artery pressure was dramatic, more than 50% in 6 hours, peaked at 6 hours with stepwise reduction, and no reduction in systemic arterial pressure occurred. Regarding the second patient, although the pulmonary artery wedge pressure was unobtainable, pulmonary venous hypertension (Group II in the WHO classification) was suspected; contribution from chronic obstructive pulmonary disease and multiple myeloma could not be excluded. This patient is even more interesting because an inhaled agent that vasodilates pulmonary arties may have increased blood flow through pulmonary venules and increased the left heart end diastolic volume (and pressure, implicitly). On the contrary, this patient also improved her pulmonary haemodynamics and resolved shock within 10–12 hours without any effect on the oxygen saturation and without a rebound phenomenon.
The treatment modalities of advanced therapy for pulmonary hypertension are typically highly expensive. Their cost is often prohibitive. Many community hospitals and some of tertiary care facilities in the USA have no access to these treatment modalities. In these cases, patients require transfer to a pulmonary hypertension centre. Unfortunately, these patients are too unstable to be transferred. High mortality rates are accentuated by a lack of diagnosis or the non-availability of treatment. In a study of 100 adult patients with pulmonary hypertension undergoing mitral valve surgery, inhaled nitroglycerine 20 µg/kg inhalation and iloprost 2.5 µg/kg inhalation, both effectively reduced mean pulmonary artery pressure, pulmonary vascular resistance without affecting mean arterial pressure, systemic vascular resistance, and cardiac output. The same study concluded that inhaled iloprost was likely more effective than inhaled nitroglycerine.12 The greatest benefits, therefore, in the use of inhaled nitroglycerine compared iloprost are in cost and availability, as nitroglycerine is available in nearly all acute medical settings, it is substantially cheaper in comparison to iloprost.
In a community hospital setting and in cases of life-threatening right heart failure and shock not responding to simple traditional treatments, thought should be given to the use of inhaled nitroglycerine. Inhaled nitroglycerine is practical, likely to be predictable, cheap, readily available in any hospital, and does not require reconstitution. This approach will allow for treatment of shock or at least temporary stabilisation until the patient is transferred to a tertiary care facility.
This review has several limitations. Both patients were treated with sildenafil, a phosphodiesterase Type 5 inhibitor, in addition to inhaled nitroglycerine. Sildenafil, although used for the treatment of WHO Group I patients with pulmonary hypertension, it is not indicated for those with severe pulmonary hypertension. Despite this, it may be used in combination with other treatments in severe cases. Sildenafil in combination with inhaled iloprost has been shown to be effective in the treatment of severe pulmonary hypertension, possibly working together synergistically to increase nitric oxide levels and promote vasodilation.13 In theory, the authors believe that inhaled nitroglycerine may have the same synergistic effect with sildenafil. The rapid improvement of these patients following inhaled nitroglycerine administration makes the improvement unlikely to be a result of sildenafil alone; nevertheless, sildenafil would be considered a confounding variable because of its promotion of pulmonary vasodilation and lack of controls in this review. Similarly, milrinone used in the second case may also be considered as a confounding variable because of its ability to also promote vasodilation and improve contractility. Milrinone alone is not indicated for treatment of severe pulmonary hypertension, although it may be used as an adjunct therapy.14 Milrinone, although on its own unlikely to effectively treat severe pulmonary hypertension, may also have promoted pulmonary vasodilation, either alone or in combination with the other pharmaceutical interventions used in the second case. In addition to the limited evidence for the use of inhaled nitroglycerine, nitroglycerine may also cause methemoglobinaemia as a result of the production of nitric oxide molecules and oxidised species. Care must be taken to monitor and evaluate these patients for this condition.
Certainly, a clinical trial would be helpful to shed light on more potential side effects, the presence or absence of a rebound phenomenon, duration of effect, and head-to-head comparison to other therapy. Other areas that need to be studied are the outpatient use and the use in Class II patients since they constitute the majority of pulmonary hypertension cases and thus inhaled nitroglycerine could be used as a nonspecific acute treatment of pulmonary hypertension of any class and may replace intravenous nitroglycerine and inhaled nitric oxide in the algorithm for treating shock due to right ventricular failure.