Abstract
Objective: This systematic review aims to evaluate the relationship between ultra-processed food (UPF) consumption and the incidence of depression among adults. It focuses on the effects of dietary intake of UPF, characterised by high levels of additives and low nutritional value, on mental health outcomes.
Method: Following the Population, Intervention, Comparator, and Outcome (PICO) framework, the population was defined as adults, the intervention as UPF consumption, and the outcome as the risk of depression. A comprehensive search was conducted across six electronic databases: PubMed, PubMed Central, Cochrane, Google Scholar, PLOS One, and ScienceDirect, adhering to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Studies published from 2019–2023 were selected based on predefined inclusion and exclusion criteria. Duplicate entries were removed using Endnote™ (Clarivate, London, UK), and data extraction was standardised using Covidence (Veritas Health Innovation Ltd, Melbourne, Australia). The quality of the studies was assessed using the Critical Appraisal Skills Program checklist.
Results: Nine studies with a combined sample of 79,701 participants were included. UPF consumption showed a consistent positive association with depression. Cohort studies reported that individuals in the highest UPF intake category had a 20–50% higher risk of developing depressive symptoms (e.g., hazard ratio: 1.22–1.52; 95% CI: 1.10–1.68). Mechanistically, findings highlighted UPF-induced gut dysbiosis, neuroinflammation, and disrupted neurotransmission as potential mediators.
Conclusions and Relevance: This systematic review concludes that increased UPF consumption is significantly associated with a higher risk of depression among adults. These results highlight the necessity of public health campaigns to lower UPF consumption and encourage better eating habits. Clinicians and policymakers should consider these associations when developing dietary guidelines and interventions to improve mental health outcomes.
Key Points
1. This systematic review examined the association between ultra-processed food (UPF) consumption and the risk of depression in adults, analysing nine studies with a total of 79,701 participants.2. Individuals with higher UPF intake demonstrated a 20–50% greater risk of developing depressive symptoms (hazard ratio: 1.22–1.52; 95% CI: 1.10–1.68).
3. The findings emphasise the need for public health strategies that reduce UPF consumption and integrate dietary guidance into mental health prevention efforts.
INTRODUCTION
Depression, also known as major depressive disorder (MDD), is marked by a loss of interest or pleasure in activities and persistent feelings of sadness and hopelessness.1 The condition affects around 280 million people globally, including 3.8% of adults and 5.7% of those over 60 years of age.1
Depression is a significant factor in the link between low nutritional quality and mental health issues, contributing to declines in quality of life and early mortality.2 Although anxiety and depression are common chronic conditions, there are no evidence-based primary prevention and treatment options based on dietary adaptation in psychiatry, which modulates biological processes.3 There is a study showing that, despite significant advancements in psychotherapy and pharmacotherapy, they only prevent half of the illness load, and only one in three mood disorders respond well to traditional treatment.4 This indicates the need for additional approaches to both prevent and cure mental diseases.
Research from nutritional psychiatry suggests that dietary quality can moderate the risk of mental diseases like depression and anxiety, which are positively correlated with unhealthy, high-fat, sugar-rich diets.5 Monteiro et al.6 introduced the NOVA method for classifying foods, which divides foods into four classes according to industrial processing. This system considers biological, physical, and chemical techniques used in food production, including additives. The groups are unprocessed; processed culinary ingredients; processed foods containing salt, oil, sugar, or other substances; and ultra-processed foods (UPF), which are primarily or entirely derived from food and additives.6 The NOVA classification system, widely used in nutritional research, is debated for its functionality and robustness, but its widespread implementation enhances comparability and accessibility.
‘Ultra-processed’ refers to ready-to-eat products made entirely or primarily from industrial materials and additives, with high profitability.7 These are becoming more popular worldwide, and consumption of these foods has been linked to internalising symptoms, anxiety, mental illnesses, and depression.3 The introduction of refined carbohydrates in the Western world in the second half of the 20th century led to industrialised foods, which has been linked to insulin resistance, cognitive decline, and dementia, potentially promoting insulin-related cognitive impairment.8
METHODOLOGY
Data Collection and Search Strategy
With the help of the supervisor, the authors formulated a search strategy, which was used to begin the systematic review in March 2023. PubMed, PubMed Central, Cochrane, Google Scholar, PLOS One, and ScienceDirect were all searched for relevant material. The following methodology was used to carry out the search strategy.
Establishing keywords and key terms
Keywords and key terms were identified in searching the identified databases for “ultra-processed foods,” “ultra processed food,” “mental disorder,” “common mental disorder,” “mood disorder,” “depres,” and “anxie.” The search terms were combined using Boolean operators, which were helpful for consolidating and refining particular search terms (Supplementary File 1).
Eligibility Criteria
Following the identification of search phrases, the authors used more search filters to focus the search and facilitate the finding of pertinent articles. The following criteria were used to select studies for this analysis: 1) quantitative observational studies (cohort, case-control, or cross-sectional); 2) persons above the age of 18 years; 3) English-language publications; and 4) within the previous 5 years. Excluded studies were 1) non-observational study designs (e.g., reviews, commentaries, editorials, interventional trials, and animal studies; 2) those with population under the age of 18 years; 3) those carried out prior to the last 5 years; or 4) those that used COVID-19 as a factor.
Selection Process
After applying screening filters for inclusion eligibility and conducting the final search, the researchers used ‘AND;’ to integrate all of the thoughts to further enhance the search results. The remaining articles were imported into Endnote™ (Clarivate, London, UK) and were screened for duplicates. All the investigators collectively screened every article. The relevant articles were sought for retrieval and then the full text of the articles was scrutinised individually for eligibility.
Data Extraction and Synthesis
The final articles were uploaded into Covidence software for data extraction purposes.9-17 Each investigator reviewed three articles primarily as well as six articles primarily reviewed by other investigators using Covidence (Appendix 1). The following data was extracted from the included articles: study ID, title, lead author, contact details, country of study, aim of study, study design, year of publication, study funding, conflict of interests, population, inclusion and exclusion criteria, method of recruitment, total number of participants, baseline characteristics (age, female %, BMI, frequency), relation of food, and impact on mental health. Critical appraisal was done using the Critical Appraisal Skills Programme checklist tool.
Data Analysis Strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (Supplementary File 2) and the ‘best fit’ framework synthesis were used to analyse the data. The best fit framework consists of the following steps: systematically finding pertinent primary research studies; using a search strategy to find relevant publications; extracting data based on quality-related characteristics; conducting framework analysis on the evidence; and creating a new framework made up of a new and old theme backed by the evidence. The key study additionally took advantage of the primary articles that were chosen from the scanning search and developed a comprehensive search strategy that included relevant keywords and therapeutic topics.
In the analysis, the authors employed two approaches, Eertmans, Baeyens, and Van Den Bergh’s model and the microbiota-gut–brain axis theory, as complementary frameworks to achieve the study’s aims. Eertmans, Baeyens, and Van Den Bergh18 presented the model of food intake and choice, highlighting a number of variables that affect eating habits. One of the internal variables is the sensory characteristics of eating. Information, the social setting, and the physical surroundings are some examples of external variables. The connections between these variables, food preferences, and eating habits are shaped by processes like social learning, Pavlovian conditioning, and simple exposure. As they are convenient (long-lasting, ready-to-eat, or heatable), hyper-palatable (incredibly delicious), highly profitable (low-cost ingredients), and made to replace all other food groups with the help of eye-catching packaging and aggressive marketing, these highly processed food products are therefore preferred over other healthier food items.
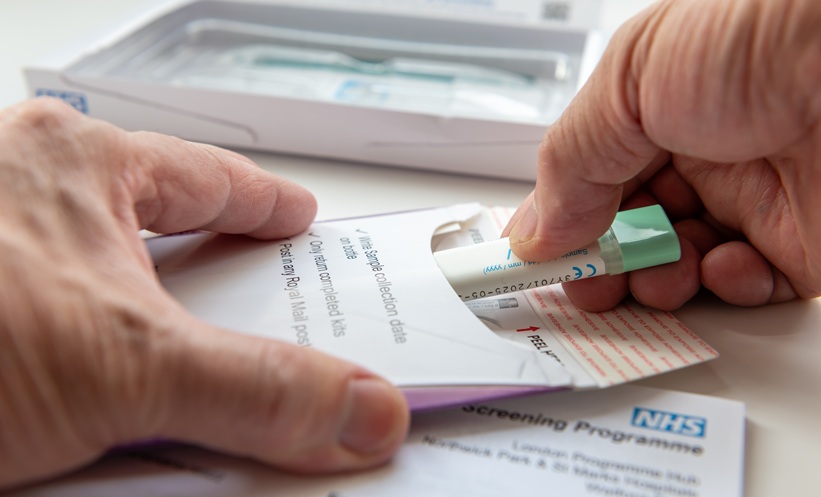
The microbiota-gut–brain axis theory (Figure 1) is used to validate the critical role that the gut microbiota plays in the two-way communication between the gut and the brain.19 It is possible that gut microbes influence neural development, modify neurotransmission, and change behaviour, all of which could contribute to the aetiology and/or progression of a number of neurological, neuropsychiatric, and neurodevelopmental disorders. While the authors primarily used existing frameworks, they remained open to emerging themes and developing new framework components where necessary. Thus, combining the two theories establishes the connection of increased incidence of depression in high UPF consumers.
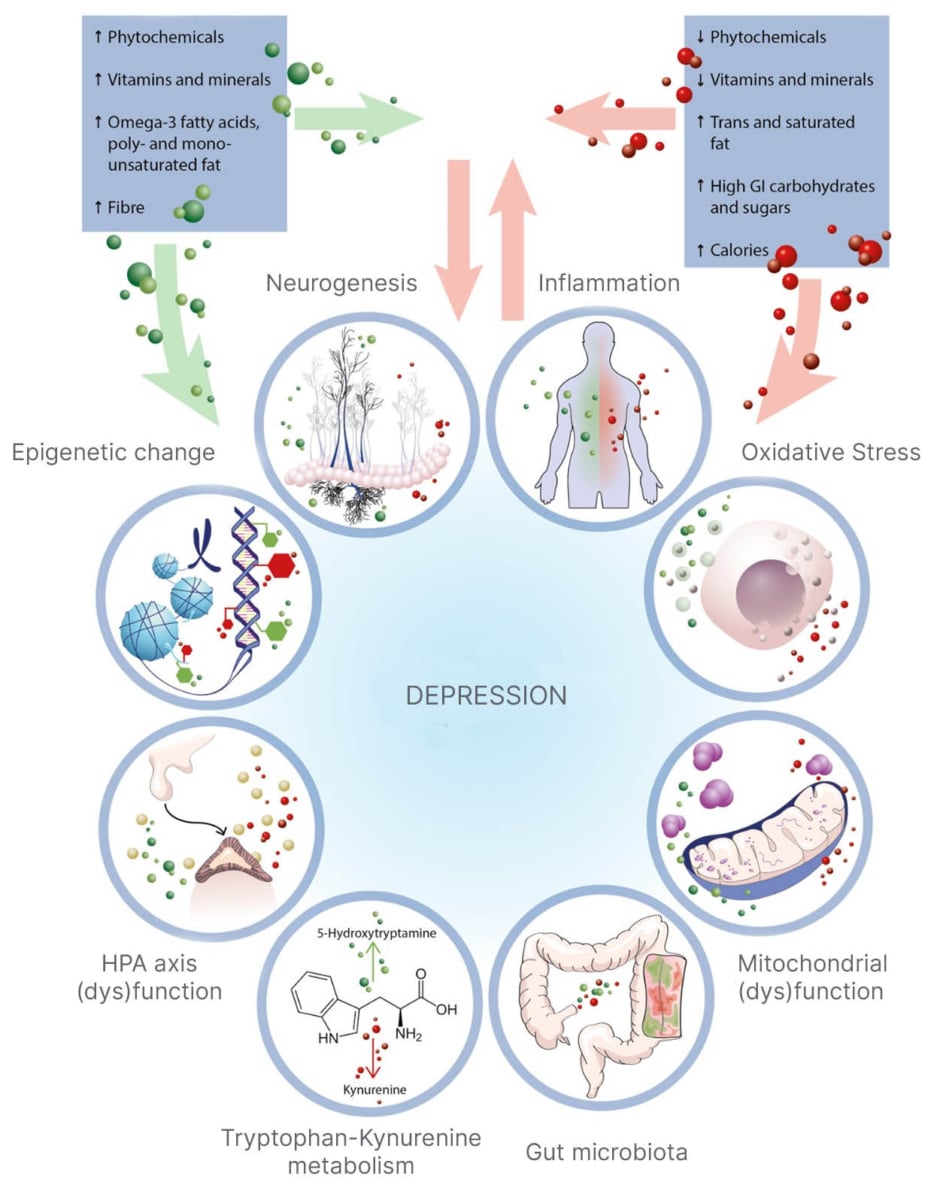
Figure 1: Microbiota-gut–brain axis theory.19
The diagram illustrates the pathways linked to depression, with conflicting eating trends affecting consumption. Green arrows indicate helpful modulation, while red arrows suggest potentially harmful ones.
GI: glycaemic index; HPA: hypothalamic-pituitary-adrenal.
RESULTS
Study Selection
The studies were chosen by screening the titles and abstracts, after which each possibly relevant full-length article was evaluated separately. Research that didn’t fit the requirements was eliminated. The initial search yielded 110 articles. Eleven duplicate articles were removed and 99 articles were subjected to screening for titles and abstracts. Eighty-three were not related and therefore excluded, and the remaining 16 articles were sought for retrieval. Two articles could not ultimately be retrieved, so the other 14 articles were assessed for eligibility. Five articles were then eliminated because of the following reasons: they discussed mental health disorders other than depression, and the study design was incorrect. Overall, nine articles were included in this review. The PRISMA flowchart illustrates the details of the selection (Figure 2).20
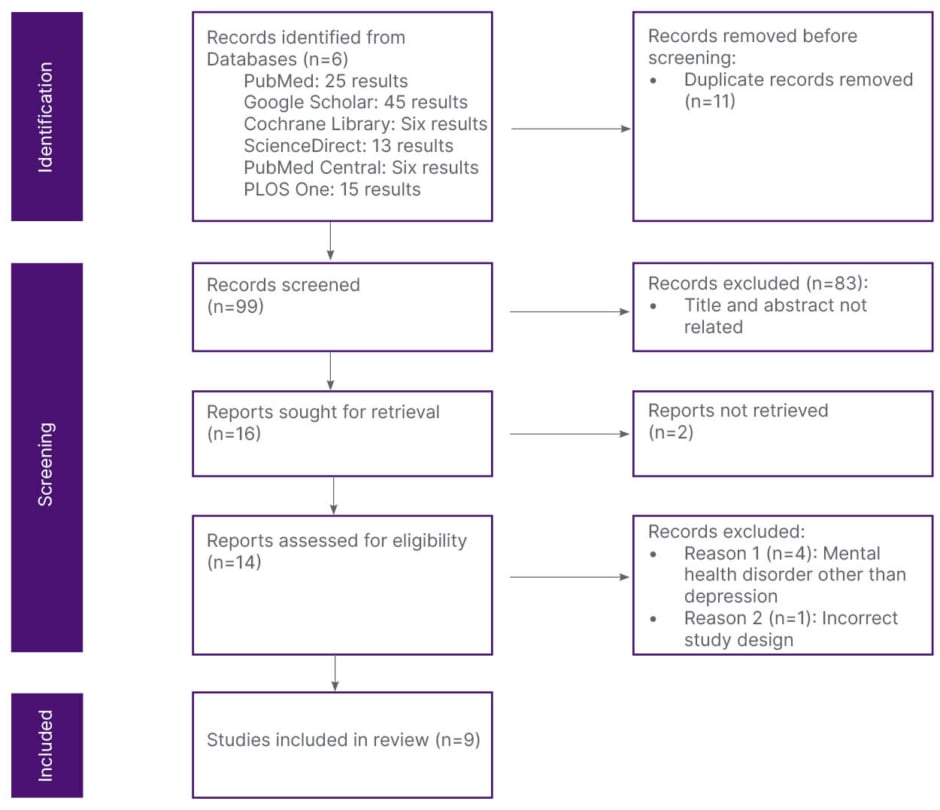
Figure 2: Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram illustrating the process of study identification, screening, eligibility assessment, and inclusion in the systematic review.
Adapted from Page et al.20
Study Characteristics
Ultimately, 79,701 participants from nine qualifying studies were included in the review. The range of sample sizes was 152–23,299 individuals. The included studies explored the connections between depression and UPF consumption. A total of five cohort and four cross-sectional designed studies were included. Eligible studies were conducted in Spain, the USA, Italy, France, Canada, South Korea, Australia, and London, UK. These studies included adult participants. The ages ranged from 20s to 60s. Some participants were recruited voluntarily (four studies), some were clinic patients (two studies), and others were recruited from social media campaigns (one study), university websites (one study), and surveys (one study).
Diet information was collected via a food frequency questionnaire in five studies12-16 and the Canadian Diet History Questionnaire II (C-DHQ II) by one study,10 while dietary recall interviews were used in two studies and a web-based dietary record platform was used by another.9,11,17 In four investigations, the Patient Health Questionnaire-9 (PHQ-9) was used to measure depressive symptoms,9-11,15 and the Center for Epidemiological Studies Depression (CES-D) Scale was used in three studies.14,16,17 The Kessler Psychological Distress (K10) scale was utilised in one study and the remaining study used the clinical diagnosis of depression.12,13
The characteristics of the nine included studies are summarised in Supplementary Table 1. These studies varied in design, sample size, and geographic distribution, but consistently assessed UPF consumption using the NOVA classification. Depression outcomes were measured using validated screening tools. Most cohort studies demonstrated longitudinal associations, while cross-sectional studies highlighted concurrent relationships between higher UPF intake and depressive symptoms. More detail can be found in [/hl]Appendix 1[/hl].
Quality Assessment
Using the Critical Appraisal Skills Programme checklist, all included studies were critically appraised for methodological rigour, clarity of objectives, validity of results, and relevance to the review question (Supplementary File 1).
Among the nine included studies, five were rated high quality, three moderate quality, and one low quality due to limitations in confounder adjustment and participant selection. Most studies demonstrated clear aims, appropriate study designs, and valid outcome measures. Common methodological strengths included the use of validated dietary assessment tools (e.g., food frequency questionnaires) and standardised depression screening scales (e.g., PHQ-9, CES-D).
However, several cross-sectional studies showed limited generalisability due to self-reported dietary data and potential recall bias. Overall, the evidence base was judged to be of moderate-to-high quality, providing reasonable confidence in the observed association between UPF consumption and depression risk (Supplementary Table 2).
DISCUSSION
A comprehensive analysis of the relationship between eating UPFs and the risk of depression was carried out. The review correlated papers with an evolving framework, which combined Eertmans, Baeyens, and Van Den Bergh’s model with the microbiota-gut–brain axis theory. The bidirectional approach ensured a theoretically sound and empirically supported framework. The review synthesised findings from relevant papers, identifying areas of agreement and disagreement, to develop a nuanced understanding of how UPF consumption correlates with depression risk.
According to a recent study, an increased risk of depression is linked to higher UPF intake, especially in artificial sweeteners and beverages. Purinergic transmission in the brain may be triggered by artificial sweeteners, and this could contribute to the aetiopathogenesis of depression, according to recent experimental findings.21 UPF food additives, like emulsifiers and artificial sweeteners, can cause biochemical alterations linked to mental illness symptoms, including reduced glucose tolerance, inflammatory mediators, oxidative stress, neuroinflammation, and changes in neurotrophic growth factor expression (Figure 3).22 According to European prospective cohort studies, people with high added sugars, high glycaemic index, and deficient nutrients are at an increased risk of developing anxiety and depression.23
Figure 3: Ultra-processed food induced gut dysbiosis and its effect on the brain.22
5-HT: 5-hydroxytryptamine; ACTH: adrenocorticotropic hormone; BBB: blood–brain barrier; CRH: corticotropin-releasing hormone; EEC: enteroendocrine cell; FFAR: free fatty acid receptor; GLP-1: glucagon-like peptide-1; HPA: hypothalamic-pituitary-adrenal; LPS: lipopolysaccharide; PYY: peptide tyrosine tyrosine; SCFA: short-chain fatty acid.
Ultra-Processed Food
As mentioned earlier, food items are divided into four classes using the NOVA classification system. UPF, which is produced using materials that have been extracted from food, food ingredients, or intentionally synthesised from food substrates or organic sources, makes up the fourth category.24 UPFs are produced using ingredients that are either cosmetic additives that make the finished product palatable or hyper-palatable, or compounds that have no or very little culinary use. These ingredients can either offer pleasing sensory qualities or mask undesired sensory qualities caused by ingredients, methods, or packaging. Colours, emulsifiers, salts, sweeteners, thickeners, flavours, taste enhancers, and anti-foaming agents are a few types of cosmetic additives.25
The consumption of visually appealing food in middle-income Asian nations is increasing due to urbanisation, labour market trends, and rising earnings. This is driven by the need for convenience foods as economies develop. Chronic diseases can result from a diet high in fat, cholesterol, sugar, processed carbs, and low in fibre and polyunsaturated fatty acids, combined with a more sedentary lifestyle (Figure 4).26 Studies show that increased use of UPFs in rich and middle-income nations is linked to negative health outcomes due to their poor nutritional profile, increased glycaemic load, and decreased gut–brain satiety signalling.27
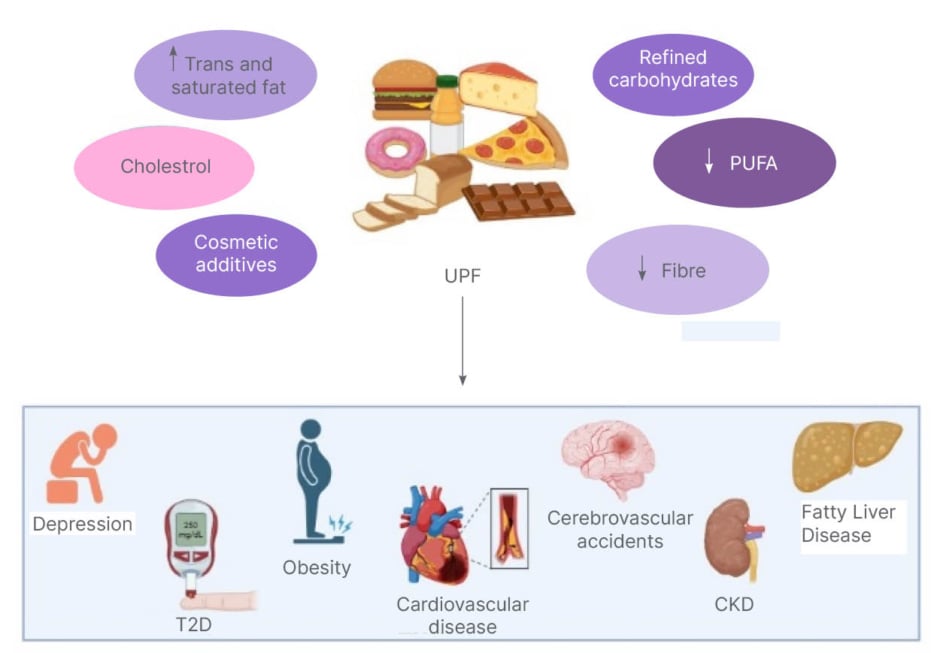
Figure 4: Health risks linked to ultra-processed food consumption.
UPF consumption and associated comorbid UPF consumption is characterised by lower dietary quality, unhealthy fats, added sugar, salt, artificial sweeteners, and food additives, which results in an increased risk for diabetes, obesity, cardiovascular disease, cerebrovascular accidents, non-alcoholic fatty liver disease, and CKD.
Created with BioRender.com.
CKD: chronic kidney disease; PUFA: polyunsaturated fatty acid; T2D: Type 2 diabetes; UPF: ultra-processed food.
The cohabitation of undernutrition and overweight, obesity, and diet-related non-communicable diseases is known as the double burden of malnutrition, and it has become a problem in many nations.22 UPF causes alterations in the physical properties of food through processing, carcinogen contamination, industrial food additives, dysbiosis of the gut microflora, increased intestinal permeability, inflammation, and endocrine disruption from chemical plasticisers used in food packaging.27
Microbiota-Gut–Brain Axis
The gut microbiota in the intestines profoundly regulates human physiology, including digestion, metabolism, and immunity, and has a strong link with nervous system diseases. Diet contributes significantly in altering the composition of gut microbiota, which either promotes or restricts the growth of specific species and results in an imbalance referred to as dysbiosis. The gut–brain-microbiota axis is a two-way communication between the enteric and central nervous systems (CNS) that links digestive processes to the brain’s emotional and cognitive centres.28 Thus, the CNS can control gastrointestinal function, and the gut can control emotional activity in the CNS. Studies show that the gut microbiota of depressed individuals significantly differs from that of healthy individuals. From the existing data, the authors can conclude that intestinal bacteria can react with the nervous system and result in depression (Figure 3).28-30
Impact on Neuropsychiatry
Around 53% of individuals who consumed UPF many times a day experienced distress or battling their mental health compared to only 18% of those who seldom or never consumed UPF, representing a three-fold increase.31 The mood and cognitive dysfunction components of neuropsychiatric illnesses have historically been linked to a dysregulation of neurotransmitters such as glutamate, serotonin, norepinephrine, and dopamine.32 Recent studies have explored the biosynthesis of gut microbiome-derived neurotransmitters, including γ-aminobutyric acid (GABA), serotonin, dopamine, and norepinephrine, which may affect the stability of the HPA axis.33 A greater number of research suggests a reciprocal relationship between the gut bacteria and the hypothalamic-pituitary-adrenal (HPA) axis. Because of how it affects cortisol release, the HPA axis is important in the pathophysiology of depression. Patients with MDD had considerably higher cortisol levels than healthy volunteers. Elevated cortisol levels have been shown to affect verbal and working memory, which lowers depression-related cognitive function. It has been demonstrated that the hippocampus, whose volume is markedly diminished in MDD, oversees the HPA axis and neurogenesis.34
Other Associations
A lot of studies have shown that excessive use of UPF is linked to increased risk of developing health issues, such as Type 2 diabetes, obesity, cancer, heart and brain disease, cognitive decline, chronic renal disease, and death from all causes. According to the meta-analysis, for every 10% increase in total UPF consumption there is a 12% (95% CI: 10–13%) increased risk of developing Type 2 diabetes secondary to insulin resistance, obesity, and systemic inflammation.35 Overconsumption of UPF can cause inflammation, cardiometabolic problems, and chronic noncommunicable illnesses including diabetes, obesity, heart disease, and cancer, including pancreatic, breast, and colorectal cancers.36,37 There is a strong association between these conditions.38 A substantial correlation exists between UPF and the gut–brain axis. Reduced hippocampal size, which is connected to obesity, diabetes, hypertension, and poor diet, is linked to reduced neuroplasticity and cognitive impairment.39 Due to severe pathophysiological reasons, overuse of UPFs might harm the kidneys and raise the risk of chronic kidney disease related to advanced glycation end products found in UPFs.40 UPF consumption has been linked to the development of non-alcoholic fatty liver disease by low quality dietary fat, low quality of carbohydrates, and dietary components promoting dysbiosis and leaky gut syndrome (Figure 4).41 A sub analysis conducted by DeVito G, Sheean P using a large European cohort also revealed that UPF consumption was significantly and positively associated with head and neck cancer (hazard ratio [HR]: 1.21; 95% CI: 1.15–1.35), oesophageal adenocarcinoma (HR: 1.21; 95% CI: 1.05–1.39), and hepatocellular carcinoma (HR: 1.23; 95% CI: 1.07–1.42).42
The search was limited to studies that only explored the risk of developing depression in UPF consumers. This review focused on studies from 2019–2023 to reflect recent evidence regarding the NOVA classification. However, this limited scope might overlook earlier foundational studies and some non-indexed publications. The review also only utilised six databases, omitting Embase, PsycINFO, and Scopus, which could lead to selection bias. Future reviews should aim to include a wider range of databases and longer timeframes for a more thorough synthesis. Secondly, the study aimed to provide in-depth insights into consumers’ experiences and perceptions through qualitative studies. Systematic reviews were excluded to avoid duplication, and the authors focused on studies from the last 5 years to include the most recent information in this rapidly evolving field. Thirdly, all the articles that did not use NOVA classification were excluded. Finally, to eliminate the difficulties that can arise from translation, all of the papers chosen for this study were published in English.
CONCLUSION
In conclusion, data that is currently published in the literature affirm that having a diet high in UPFs increases the chance of developing depression. This association remains significant even after adjusting for potential confounders. Consumption of UPF is linked to a decline in diet quality, with negative correlations with fibre and protein and positive correlations with sugar, fat, and saturated fat. The authors’ findings point to a potential relationship between UPF consumption and risk of developing depression. However, considering the limitations of the NOVA classification system and the complex, multi-cause nature of depression, it is critical to take into account other contributing factors such as genetics, environment, and lifestyle.
These results have important ramifications for public health, particularly for food policymakers who ought to discourage the use of UPF and encourage the consumption of fresh, less processed foods. More practical dietary recommendations should be developed by concentrating on how ultra processing alters the characteristics of whole meals and how these foods impact the gut microbiota.