Abstract
Physical inactivity is a global health problem that contributes to the increasing risk of obesity and diabetes. Wearable devices are defined as technologies that can be comfortably worn on the body and that are designed to be effective at improving the health and overall fitness of the wearer. The aim of this narrative review is to summarise the current studies investigating the efficacy of wearable devices, especially mobile applications, for the management of diabetes. The use of pedometers or accelerometers has been shown to increase physical activity by approximately 1 hour per week; however, rates of obesity and diabetes were not affected. Although recent assessments of the effect of smartphone applications on physical activity and glycaemic control are sparse, they are useful for promoting physical activity and for treating diabetes. The interactions with patients using wearable devices for self-monitoring, education, and coaching are essential for the improvement of diabetes. However, there are currently no clinical trials investigating the efficacy of the ‘perfect’ wearable device, whereby patients with diabetes can accurately and comfortably monitor their physical activity, energy balance, blood pressure, heart rate, and blood glucose level. Analysis of big data from wearable device users will contribute to the development of effective wearable devices. Developments in wearable technology are anticipated and further studies will be required to assess the efficacy of wearable devices in measuring and promoting physical activity in the management of diabetes.
INTRODUCTION
In 2016, a smartphone game application, Pokémon GO, was released. The game encourages users to walk and explore their surroundings, using their mobile device’s global positioning system, with the aim of catching Pokémon, which are typically located in public areas. Howe et al.1 reported that playing Pokémon GO was associated with a moderate increase in daily physical activity; however, the increase in activity was no longer observed 6 weeks after installation of the game. Although the positive effect of Pokémon GO on physical activity tends to taper off, it is an important example of how to promote health, specifically increasing locomotive physical activity via a smartphone application.2 Physical inactivity is a global health problem responsible for the increasing risk of obesity and non-communicable diseases, such as diabetes, coronary heart disease, and breast and colon cancers. By increasing physical activity, the life expectancy of humans is expected to rise by 0.68 years.3 Increasing physical activity is the cornerstone of obesity and diabetes management, two conditions that are now worldwide public health epidemics. Not only regular exercise, but also daily physical activity, is important for the prevention and management of obesity and diabetes;4,5 therefore, it is essential for clinicians to measure and promote physical activity in individuals with these conditions.
There are many electronic technologies and computers that can comfortably be worn on the body and perform many tasks in conjunction with hand-held devices such as smartphones.6 For example, commercially available wearable devices use applications to monitor vital signs and physical activity. However, there are challenges to the development of simple and powerful applications for medical use, and wearable health monitoring systems are becoming important for long-term health management, playing a pivotal role in the health of the elderly population.7 Chen et al.8 designed ‘smart clothing’ that incorporates mobile applications, cloud computing, and big data analytics in a wearable health monitoring system. The smart clothing includes a vital sign monitor, ECG, electroencephalogram, and blood oxygen monitor. It is clear to see that wearable devices, such as smart clothing, will have a large impact on healthcare.
While there is still no perfect wearable device for measuring physical activity, pedometers, accelerometers, and smartphone applications can be regarded as prototypic wearable devices. Although a systematic review and meta-analysis has shown that interventions using computer, mobile, and wearable technology tools reduce sitting time by approximately 40 minutes per day,9 the feasibility, acceptability, and effectiveness of mobile-based technology to promote active lifestyles in individuals with Type 2 diabetes mellitus (T2DM) are inconclusive.10 The focus of this review is to summarise the current studies investigating the efficacy of wearable devices (including pedometers, accelerometers, and mobile applications) for the management of diabetes and to discuss the future prospects for using wearable devices in clinical care.
PEDOMETERS AND ACCELEROMETERS
Pedometers are simple physical activity monitoring devices that display step count and are used by many people for health and fitness. Accelerometers were first developed in the 1980s and have been used extensively for measuring physical activity under free-living conditions. Recently developed accelerometers can characterise activity patterns (i.e., locomotive or non-locomotive movements) in addition to estimating physical activity and energy expenditure.11 There have been a number of studies investigating the efficacy of pedometers and accelerometers for the management of diabetes, and randomised controlled trials (RCT) have also been conducted to investigate the usefulness of pedometers and accelerometers in patients with diabetes.12-16 Baskerville et al.17 assessed the impact of pedometers and accelerometers on physical activity and HbA1c levels in patients with T2DM. This systematic review and meta-analysis analysed nine pedometer studies and three accelerometer studies. The use of these devices increased free-living physical activity by approximately 1 hour per week; however, no significant effects were observed in BMI, HbA1c levels, blood pressure, or lipid profile in patients with T2DM. The heterogeneity between study duration and the types of pedometers and accelerometers used was a limitation of this meta-analysis, as well as the fact that all study subjects were physically active, with normal glycaemic control (average HbA1c: 7.6%) or progressed diabetic complications. However, these results indicate that physical activity monitoring (wearing pedometers and accelerometers) may be insufficient for improving diabetes. In addition, although there were strong correlations between accelerometer and pedometer-measured steps per day,18 accelerometers can detect more steps than pedometers19,20 and pedometers may not be suitable for monitoring daily physical activity in frail older individuals with slow gaits.20 Some studies recommend the use of pedometers in normal-weight individuals, whereas accelerometers are more suitable for obese individuals.21 On the other hand, accelerometer-measured sedentary time was unfavourably associated with insulin sensitivity and triglycerides in cross-sectional data.22 It is important to give individual feedback on physical activity data and instructions to patients for the management of diabetes, and the interaction with patients using smart devices will be required to achieve sufficient clinical effects.
SMARTPHONE APPLICATIONS AND WEARABLE ACTIVITY TRACKERS
In 2017, the percentage of people who used a smartphone was 77% in the UK, 78% in the USA, and 64% in Japan.23 Considering the large number of smartphone users, interventions using electronic health (eHealth) and mobile health (mHealth) strategies are a promising way to promote physical activity. Several systematic reviews and meta-analyses have reported that internet-delivered intervention,24 social media,25 and smartphones26 are useful for increasing daily physical activity. Moreover, eHealth and mHealth strategies may also be effective for improving obesity and diabetes outcomes: mobile phone application-based interventions were associated with a reduction in body weight (-1.04 kg) and BMI (-0.43 kg/m2). Thomas et al.27 also reported that a commercial programme for treating obesity, named Weight Watchers Online, could effectively reduce body weight in obese individuals, whereas participants with activity tracking devices did not achieve an additional increase in physical activity. However, the efficacy of eHealth and mHealth in increasing physical activity in patients with diabetes has not been fully investigated.
The author searched English literature using PubMed/MEDLINE and EMBASE. To identify potential studies the following search terms were used: “diabetes,” “smartphone” or “wearable device,” “physical activity” or “exercise,” and “randomized controlled trial.” Studies were included if they met the following criteria: study subjects were ≥18 years of age and were diagnosed as having diabetes or prediabetes, the study was a randomised controlled trials, and the study duration was ≥12 weeks. Four studies were eligible (Table 1).28-31
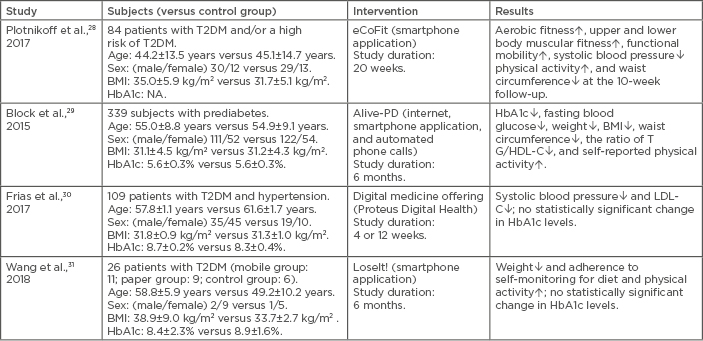
Table 1: Randomised controlled trials investigating the efficacy of a smartphone application and wearable activity tracker for the management of diabetes.
↑: increased; ↓: decreased; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; NA: data not available; T2DM: Type 2 diabetes mellitus; TG: triglyceride.
Plotnikoff et al.28 assessed the efficacy of an innovative lifestyle programme named eCoFit to improve health and fitness in patients with T2DM. The eCoFit application consists of workout circuits (eCoFit Challenge), self-monitoring functions (Fit Mind Challenges), and a link to social media (Facebook). This application instructs users where and how to increase physical activity in the city of Newcastle upon Tyne, UK, and integrates aerobic exercise and resistance training using the outdoor environment in the city. Aerobic fitness (evaluated using the single stage submaximal treadmill walking test), lower body muscular fitness (evaluated using the chair stand test), upper body muscular fitness, and functional mobility were all improved after 10 weeks of intervention. Physical activity also increased by an average of 1,330 steps per day, while waist circumference (-2.8 cm) and systolic blood pressure (-10.4 mmHg) were reduced. Moreover, aerobic fitness, lower and upper body muscular fitness, functional mobility, waist circumference (-2.14 cm), and systolic blood pressure (-11.3 mmHg) improved in the study subjects compared with the controls at the 20-week follow-up. However, no significant differences in physical activity, diastolic blood pressure, or BMI were observed between the groups. The retention rate was 71% at the 20-week follow-up. This RCT suggests that intervention using a smartphone application and social media has the potential to increase physical activity in patients with T2DM. The eCoFit is also unique in its practicality in locating places to exercise in the public space. However, the study participants were relatively young and might have been more motivated to engage in physical activity than typical patients with T2DM. The generalisability of the results remains to be tested.
A fully automated, tailored, online behavioural change programme using a mobile phone application can effectively improve glycaemic control and obesity, although it does not monitor physical activity continuously.29 The Alive-PD provides a 1-year programme for the prevention of diabetes and includes individually tailored goal setting and other activities that are supported by the internet, email, and a mobile phone application. Participants set goals of 150–300 minutes of aerobic exercise per week based on their self-reported physical activity level at baseline, and the programme recommends personally achievable small-step goals of dietary and physical activity habits. In addition, Alive-PD provides tools for tracking diet, physical activity, and weight; health information on diabetes; virtual social support; feedback on diet and physical activity; and weekly reminders. Furthermore, Alive-PD has a point system with monetary rewards and team competition, promoting engagement and retention. The retention rate was 86.1% at the 6-month follow-up assessment. The mean reduction in fasting glucose level was greater in the Alive-PD group (-7.36 mg/dL) compared with the control group (-2.19 mg/dL), as was the mean reduction in HbA1c level (-0.26% and -0.18%, respectively). Body weight, BMI, and the ratio of triglycerides to high-density lipoprotein cholesterol were all also significantly reduced in those taking part in the programme. Furthermore, after a 6-month intervention, the Framingham 8-year diabetes risk was reduced from 16% to 11%. Self-reported physical activity, dietary habits, sleep, fatigue, and self-confidence were improved. Therefore, this internet and mobile-based programme was clinically effective at preventing the incidence of diabetes and these results show that eHealth and mHealth strategies can be a valuable tool for diabetes prevention and management.
A recent RCT conducted in the USA by Frias et al.30 investigated the effect of a digital medicine offering that measures physical activity using medication taken with an ingestible sensor, wearable sensor patches, and a mobile application. Patients with uncontrolled hypertension and T2DM were enrolled in a 12-week RCT. The ingestible sensor is activated when the patients take a pill, which sends a specific signal that is detected by the wearable sensor patch. Patient information is recorded and transmitted to a mobile application, secure cloud storage, and a web portal. All clinical data are used by the healthcare team, and the investigators review reports on the web portal, adjust medications, and provide patient education and counselling at any time. The mean adherence was 84% for 12 weeks. The digital medication offering group had a significant reduction in systolic blood pressure compared to the usual care group at Week 4 (-21.8 mmHg versus -12.7 mmHg, respectively); this reduction was maintained at Week 12 (-24.6 mmHg versus -15.2 mmHg, respectively). On the other hand, no significant difference in HbA1c reduction was observed between the digital medication offering group and controls. However, in patients with a baseline HbA1c of ≥8%, the digital medication offering group showed a significant decrease in HbA1c compared to an increase of HbA1c in the usual care group (-0.31% versus 0.26%, respectively). The change in physical activity was not measured; thus, the effect of a digital medicine offering on physical activity promotion was unknown. Nonetheless, digital medicines may improve self-care in patients with T2DM.
Wang et al.31 assessed the feasibility of the mHealth intervention and compared its efficacy with the paper-based behavioural intervention and standard care in individuals with T2DM. The participants in the mHealth group used the LoseIt! smartphone application for self-monitoring diet, physical activity, and weight loss, as well as Diabetes Connect connected with a Bluetooth®-enabled glucometer (MyGlucoHealth). This pilot study was a small-scale RCT that enrolled 26 subjects, approximately 70% of whom were African-American. The retention rates at 3 and 6 months were 96% and 92%, respectively. The median percentage of days with self-monitoring entries for diet, physical activity, weight, and glucose level were 96.6%, 37.3%, 49.7%, and 72.7%, respectively, in the mHealth intervention group; these numbers were significantly higher than those in the paper-based intervention group. The 6-month mHealth intervention decreased participants’ HbA1c levels from 8.4% to 6.9%, whereas those using the paper-based intervention had an average HbA1c level of ≥9% for 6 months; the control group exhibited no change in glycaemic control. In addition, the participants in the mHealth intervention group achieved an average weight loss of 1.8%, whereas the paper-based intervention group and controls showed weight gain. Patient adherence to self-monitoring of physical activity was low compared to their dietary monitoring. However, the adherence rate for physical activity in the paper-based intervention group was only 1.2%, which suggests that a mobile application was useful for self-monitoring of physical activity. Using mHealth tools has the potential to increase patient adherence to behavioural self-monitoring and to improve diabetes and obesity.
These studies showed that using smartphone applications could promote physical activity and help control weight, blood pressure, and lipid levels in the management of diabetes. However, no study duration was >6 months; thus, the long-term efficacy of smartphone applications for the management of diabetes is not clear.
Smartphones are useful as activity tracking devices.32,33 However, steps measured by iPhone step counts seem to be underestimated by approximately 1,340 steps per day in the free-living condition.34 Smartphone applications also underestimate changes in the time spent undertaking light-intensity and moderate-to-vigorous-intensity physical activity and overestimate changes in sedentary time with reference to an accelerometer.35 Wearable devices, including smartphone applications, can reliably measure heart rate, distance, and sleep duration; however, the measurement of energy consumption is still inaccurate.36 It is indisputable that the manufacturers of wearable devices that measure physical activity should improve their algorithms and devices for medical use.
FUTURE STUDIES
Although current evidence regarding the impact of wearable devices on the management of diabetes is limited, a number of well-designed studies are ongoing. Alonso-Domínguez et al.37 are investigating the effect of a multifactorial intervention that includes the use of a smartphone application, EVIDENT II, on changes to physical activity in primary care. In addition, Valentiner et al.38 are investigating whether 8–12 weeks of interval walking training supported by the smartphone-based InterWalk application is effective for increasing moderate and vigorous-intensity physical activity in patients with T2DM. Recently, a RCT investigating whether an mHealth intervention using a smartphone application (Pregnant+) improves glycaemic control in women with gestational diabetes has been completed.39 The primary outcome of this study focussed on the 2-hour blood glucose level during an oral glucose tolerance test; however, the secondary outcome included change in physical activity.
The DiaCert-study evaluated the effect of a 12-week smartphone application intervention aimed at increasing physical activity in Swedish patients with T2DM.40 It is noteworthy that physical activity and sedentary behaviour were measured by the wGT3x-BT triaxial accelerometer (Actigraph, Pensacola, Florida, USA) in addition to counting daily steps by a smartphone application. Muralidharan et al.41 are investigating the feasibility, cost-effectiveness, and sustainability of an mHealth intervention programme (mDiab) in individuals at high risk of T2DM in India. The mDiab programme involves 12 weeks of video lessons for diabetes prevention, tracking of lifestyle behaviours, and weekly communication with health coaches. The outcomes include weight loss, changes in physical activity, diet, quality of life, and cardiometabolic risk factors. This RCT focusses on the prevention of T2DM in individuals with prediabetes and/or obesity.
Exergaming is a novel approach to increase physical activity (e.g., Pokémon GO). Höchsmann et al.42 developed a smartphone-based, game-like software application and platform (MOBIGAME) specifically designed for middle-aged patients with T2DM. The players’ physical activity is responsible for their achievements in the game, and they are motivated to increase physical activity in reality. The results should indicate whether exergaming is useful for increasing physical activity in middle-aged individuals as well as adolescents. Osborn et al.43 reported that using the One Drop mobile application on iPhone and Apple Watch was associated with a reduction in HbA1c levels of 1.36%. There are many commercial smartwatches that show promise in healthcare44 and the smartwatch is the most familiar wearable device to consumers; collection and analysis of big data from real-world users will contribute to the development of a perfect wearable device.
Furthermore, artificial intelligence will play a crucial role in the development of wearable devices for the management of diabetes. Artificial intelligence methods have become increasingly important for diabetes management: blood glucose control, blood glucose prediction, detection of adverse glycaemic events, detection of meals and exercise, insulin bolus calculators, and lifestyle support in diabetes management.45 Therefore, artificial intelligence methods in combination with wearable devices will enable the creation of personalised diabetes management.
CONCLUSION
In conclusion, using smartphone applications and accelerometers or pedometers in the management of diabetes is effective for promoting physical activity, and the future of wearable device looks promising for the healthcare field. Ideally, everybody should be able to wear high-tech devices without feeling uncomfortable. For individuals with diabetes, physical activity, blood glucose level, blood pressure, heart rate, and energy intake and consumption should be objectively and accurately measured using wearable devices, such as glasses, watches, belts, and shoes, under a free-living condition. Wearable, non-invasive epidermal glucose sensors are currently under development and will improve glycaemic control and reduce the risk of complications.46 However, such wearable devices are still not routinely used and there are currently no clinical trials investigating the efficacy of the perfect wearable device for promoting physical activity and treating diabetes. On the other hand, a smartphone could be a substitute for a wearable device if users always carry it with them. In addition, in recent years, big data have become increasingly important in scientific research. Big data analysis integrates a large amount of heterogeneous data, such as demographic, physiological, biomedical, and omics (e.g., genomics, epigenomics, and metabolomics) data in medicine.47 The ehealth data recorded by wearable devices will be useful for big data analyses in the future. The results of the studies included in this review demonstrate that wearable devices have a beneficial potential for the management of diabetes. However, ideally, systematic searches and statistical evaluation should be performed to assess all the relevant studies. Therefore, it remains inconclusive whether using wearable device is truly effective for the management of diabetes and the improvement in wearable technology and further studies are required.








